| Neurobiological effects of physical exercise | |
|---|---|
| Exercise therapy – medical intervention | |
 A woman engaging in aerobic exercise (jogging) | |
| ICD-9-CM | 93.19 |
| MeSH | D005081 |
| LOINC | 73986-2 |
| eMedicine | 324583 |
The neurobiological effects of physical exercise involve possible interrelated effects on brain structure, brain function, and cognition.[1][2][3][4] Research in humans has demonstrated that consistent aerobic exercise (e.g., 30 minutes every day) may induce improvements in certain cognitive functions, neuroplasticity and behavioral plasticity; some of these long-term effects may include increased neuron growth, increased neurological activity (e.g., c-Fos and BDNF signaling), improved stress coping, enhanced cognitive control of behavior, improved declarative, spatial, and working memory, and structural and functional improvements in brain structures and pathways associated with cognitive control and memory.[5][6][7] The effects of exercise on cognition may affect academic performance in children and college students, improve adult productivity, preserve cognitive function in old age, preventing or treating certain neurological disorders, and improving overall quality of life.[8][9][10][11]
In healthy adults, aerobic exercise has been shown to induce transient effects on cognition after a single exercise session and persistent effects on cognition following consistent exercise over the course of several months.[1][7][12] People who regularly perform an aerobic exercise (e.g., running, jogging, brisk walking, swimming, and cycling) have greater scores on neuropsychological function and performance tests that measure certain cognitive functions, such as attentional control, inhibitory control, cognitive flexibility, working memory updating and capacity, declarative memory, spatial memory, and information processing speed.[5][7][12][13][14]
Aerobic exercise has both short and long term effects on mood and emotional states by promoting positive affect, inhibiting negative affect, and decreasing the biological response to acute psychological stress.[12] Aerobic exercise may affect both self-esteem and overall well-being (including sleep patterns) with consistent, long term participation.[15] Regular aerobic exercise may improve symptoms associated with central nervous system disorders and may be used as adjunct therapy for these disorders. There is some evidence of exercise treatment efficacy for major depressive disorder and attention deficit hyperactivity disorder.[9][16][17][18] The American Academy of Neurology's clinical practice guideline for mild cognitive impairment indicates that clinicians should recommend regular exercise (two times per week) to individuals who have been diagnosed with this condition.[19]
Some preclinical evidence and emerging clinical evidence supports the use of exercise as an adjunct therapy for the treatment and prevention of drug addictions.[20][21][22][23]
Reviews of clinical evidence also support the use of exercise as an adjunct therapy for certain neurodegenerative disorders, particularly Alzheimer's disease and Parkinson's disease.[24][25] Regular exercise may be associated with a lower risk of developing neurodegenerative disorders.[26]
Long-term effects
Neuroplasticity
Neuroplasticity is the process by which neurons adapt to a disturbance over time, and most often occurs in response to repeated exposure to stimuli.[27] Aerobic exercise increases the production of neurotrophic factors[note 1] (e.g., BDNF, IGF-1, VEGF) which mediate improvements in cognitive functions and various forms of memory by promoting blood vessel formation in the brain, adult neurogenesis,[note 2] and other forms of neuroplasticity.[2][5][29][30] Consistent aerobic exercise over a period of several months induces clinically significant improvements in executive functions and increased gray matter volume in nearly all regions of the brain,[31] with the most marked increases occurring in brain regions that give rise to executive functions.[1][5][6] The brain structures that show the greatest improvements in gray matter volume in response to aerobic exercise are the prefrontal cortex, caudate nucleus, and hippocampus;[1][5] less significant increases in gray matter volume occur in the anterior cingulate cortex, parietal cortex, cerebellum, and nucleus accumbens.[5] The prefrontal cortex, caudate nucleus, and anterior cingulate cortex are among the most significant brain structures in the dopamine and norepinephrine systems that give rise to cognitive control.[32] Exercise-induced neurogenesis (i.e., the increases in gray matter volume) in the hippocampus is associated with measurable improvements in spatial memory.[33][34] Higher physical fitness scores, as measured by VO2 max, are associated with better executive function, faster information processing speed, and greater gray matter volume of the hippocampus, caudate nucleus, and nucleus accumbens.[1]
Structural growth
Reviews of neuroimaging studies indicate that consistent aerobic exercise increases gray matter volume in nearly all regions of the brain,[31] with more pronounced increases occurring in brain regions associated with memory processing, cognitive control, motor function, and reward;[1][5][31] the most prominent gains in gray matter volume are seen in the prefrontal cortex, caudate nucleus, and hippocampus, which support cognitive control and memory processing, among other cognitive functions.[1][6] Moreover, the left and right halves of the prefrontal cortex, the hippocampus, and the cingulate cortex appear to become more functionally interconnected in response to consistent aerobic exercise.[1] Three reviews indicate that marked improvements in prefrontal and hippocampal gray matter volume occur in healthy adults that regularly engage in medium intensity exercise for several months.[1][35] Other regions of the brain that demonstrate moderate or less significant gains in gray matter volume during neuroimaging include the anterior cingulate cortex, parietal cortex, cerebellum, and nucleus accumbens.[5][36]
Regular exercise has been shown to counter the shrinking of the hippocampus and memory impairment that naturally occurs in late adulthood.[5] Sedentary adults over age 55 show a 1–2% decline in hippocampal volume annually.[37] A neuroimaging study with a sample of 120 adults revealed that participating in regular aerobic exercise increased the volume of the left hippocampus by 2.12% and the right hippocampus by 1.97% over a one-year period.[37] Subjects in the low intensity stretching group who had higher fitness levels at baseline showed less hippocampal volume loss, providing evidence for exercise being protective against age-related cognitive decline.[37] In general, individuals that exercise more over a given period have greater hippocampal volumes and better memory function.[5] Aerobic exercise has also been shown to induce growth in the white matter tracts in the anterior corpus callosum, which normally shrink with age.[5][35]
The various functions of the brain structures that show exercise-induced increases in gray matter volume include:
- Caudate nucleus – responsible for stimulus-response learning and inhibitory control; implicated in Parkinson's disease and ADHD[38][39]
- Cerebellum – responsible for motor coordination and motor learning[40]
- Hippocampus – responsible for storage and consolidation of declarative memory and spatial memory[39]
- Nucleus accumbens – responsible for incentive salience ("wanting" or desire, the form of motivation associated with reward) and positive reinforcement; implicated in addiction[41]
- Parietal cortex – responsible for sensory perception, working memory, and attention[38][42]
- Prefrontal and anterior cingulate cortices – required for the cognitive control of behavior, particularly: working memory, attentional control, decision-making, cognitive flexibility, social cognition, and inhibitory control of behavior;[38][43] implicated in attention deficit hyperactivity disorder (ADHD) and addiction[38]
Persistent effects on cognition
Concordant with the functional roles of the brain structures that exhibit increased gray matter volumes, regular exercise over a period of several months has been shown to persistently improve numerous executive functions and several forms of memory.[5][6][44][45] In particular, consistent aerobic exercise has been shown to improve attentional control,[note 3] information processing speed, cognitive flexibility (e.g., task switching), inhibitory control,[note 4] working memory updating and capacity,[note 5] declarative memory,[note 6] and spatial memory.[5][6][7][44] In healthy young and middle-aged adults, the effect sizes of improvements in cognitive function are largest for indices of executive functions and small to moderate for aspects of memory and information processing speed.[1][7] It may be that in older adults, individuals benefit cognitively by taking part in both aerobic and resistance type exercise of at least moderate intensity.[47] Individuals who have a sedentary lifestyle tend to have impaired executive functions relative to other more physically active non-exercisers.[6] A reciprocal relationship between exercise and executive functions has also been noted: improvements in executive control processes, such as attentional control and inhibitory control, increase an individual's tendency to exercise.[6]
Mechanism of effects
BDNF signaling
One of the most significant effects of exercise on the brain is increased synthesis and expression of BDNF, a neuropeptide and hormone, resulting in increased signaling through its receptor tyrosine kinase, tropomyosin receptor kinase B (TrkB).[4][50][51] Since BDNF is capable of crossing the blood–brain barrier, higher peripheral BDNF synthesis also increases BDNF signaling in the brain.[30] Exercise-induced increases in BDNF signaling are associated with improved cognitive function, improved mood, and improved memory.[29][50] Furthermore, research has provided a great deal of support for the role of BDNF in hippocampal neurogenesis, synaptic plasticity, and neural repair.[5][50] Engaging in moderate-high intensity aerobic exercise such as running, swimming, and cycling increases BDNF biosynthesis through myokine signaling, resulting in up to a threefold increase in blood plasma and BDNF levels;[4][50][51] exercise intensity is positively correlated with the magnitude of increased BDNF biosynthesis and expression.[4][50][51] A meta-analysis of studies involving the effect of exercise on BDNF levels found that consistent exercise modestly increases resting BDNF levels as well.[29] This has important implications for exercise as a mechanism to reduce stress since stress is closely linked with decreased levels of BDNF in the hippocampus. In fact, studies suggest that BDNF contributes to the anxiety-reducing effects of antidepressants. The increase in BDNF levels caused by exercise helps reverse the stress-induced decrease in BDNF which mediates stress in the short term and buffers against stress-related diseases in the long term.[52]
IGF-1 signaling
IGF-1 is a peptide and neurotrophic factor that mediates some of the effects of growth hormone;[53] IGF-1 elicits its physiological effects by binding to a specific receptor tyrosine kinase, the IGF-1 receptor, to control tissue growth and remodeling.[53] In the brain, IGF-1 functions as a neurotrophic factor that, like BDNF, plays a significant role in cognition, neurogenesis, and neuronal survival.[50][54][55] Physical activity is associated with increased levels of IGF-1 in blood serum, which is known to contribute to neuroplasticity in the brain due to its capacity to cross the blood–brain barrier and blood–cerebrospinal fluid barrier;[5][50][53][54] consequently, one review noted that IGF-1 is a key mediator of exercise-induced adult neurogenesis, while a second review characterized it as a factor which links "body fitness" with "brain fitness".[53][54] The amount of IGF-1 released into blood plasma during exercise is positively correlated with exercise intensity and duration.[56]
VEGF signaling
VEGF is a neurotrophic and angiogenic (i.e., blood vessel growth-promoting) signaling protein that binds to two receptor tyrosine kinases, VEGFR1 and VEGFR2, which are expressed in neurons and glial cells in the brain.[55] Hypoxia, or inadequate cellular oxygen supply, strongly upregulates VEGF expression and VEGF exerts a neuroprotective effect in hypoxic neurons.[55] Like BDNF and IGF-1, aerobic exercise has been shown to increase VEGF biosynthesis in peripheral tissue which subsequently crosses the blood–brain barrier and promotes neurogenesis and blood vessel formation in the central nervous system.[30][57] Exercise-induced increases in VEGF signaling have been shown to improve cerebral blood volume and contribute to exercise-induced neurogenesis in the hippocampus.[5][57]
Irisin
A study using FNDC5 knock-out mice as well as artificial elevation of circulating irisin levels showed that irisin confers beneficial cognitive effects of physical exercise and that it can serve an exercise mimetic in mice in which it could "improve both the cognitive deficit and neuropathology in Alzheimer's disease mouse models". The mediator and its regulatory system is therefore being investigated for potential interventions to improve – or further improve – cognitive function or alleviate Alzheimer's disease in humans.[58][59][60] Experiments indicate irisin may be linked to regulation of BDNF and neurogenesis in mice.[61]
Short-term effects
Transient effects on cognition
In addition to the persistent effects on cognition that result from several months of daily exercise, acute exercise (i.e., a single bout of exercise) has been shown to transiently improve a number of cognitive functions.[12][62][63] Reviews and meta-analyses of research on the effects of acute exercise on cognition in healthy young and middle-aged adults have concluded that information processing speed and a number of executive functions – including attention, working memory, problem solving, cognitive flexibility, verbal fluency, decision making, and inhibitory control – all improve for a period of up to 2 hours post-exercise.[12][62][63] A systematic review of studies conducted on children also suggested that some of the exercise-induced improvements in executive function are apparent after single bouts of exercise, while other aspects (e.g., attentional control) only improve following consistent exercise on a regular basis.[44] Other research has suggested immediate performative enhancements during exercise, such as exercise-concurrent improvements in processing speed and accuracy during both visual attention and working memory tasks.[64][65]
Exercise-induced euphoria

Continuous exercise can produce a transient state of euphoria – a positively-valenced affective state involving the experience of pleasure and feelings of profound contentment, elation, and well-being – which is colloquially known as a "runner's high" in distance running or a "rower's high" in rowing.[66][67][68][69] Current medical reviews indicate that several endogenous euphoriants are responsible for producing exercise-related euphoria, specifically phenethylamine (an endogenous psychostimulant), β-endorphin (an endogenous opioid), and anandamide (an endogenous cannabinoid).[70][71][72][73][74]
Effects on neurochemistry
β-Phenylethylamine
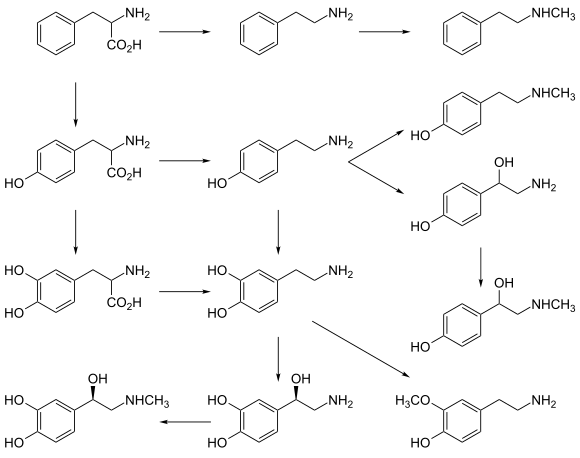
β-Phenylethylamine, commonly referred to as phenethylamine, is a human trace amine and potent catecholaminergic and glutamatergic neuromodulator that has similar psychostimulant and euphoriant effects and a similar chemical structure to amphetamine.[78] Thirty minutes of moderate to high intensity physical exercise has been shown to induce an enormous increase in urinary β-phenylacetic acid, the primary metabolite of phenethylamine.[70][71][72] Two reviews noted a study where the average 24 hour urinary β-phenylacetic acid concentration among participants following just 30 minutes of intense exercise increased by 77% relative to baseline concentrations in resting control subjects;[70][71][72] the reviews suggest that phenethylamine synthesis sharply increases while an individual is exercising, during which time it is rapidly metabolized due to its short half-life of roughly 30 seconds.[70][71][72][79] In a resting state, phenethylamine is synthesized in catecholamine neurons from L-phenylalanine by aromatic amino acid decarboxylase (AADC) at approximately the same rate at which dopamine is produced.[79]
In light of this observation, the original paper and both reviews suggest that phenethylamine plays a prominent role in mediating the mood-enhancing euphoric effects of a runner's high, as both phenethylamine and amphetamine are potent euphoriants.[70][71][72]
β-Endorphin
β-Endorphin (contracted from "endogenous morphine") is an endogenous opioid neuropeptide that binds to μ-opioid receptors, in turn producing euphoria and pain relief.[73] A meta-analytic review found that exercise significantly increases the secretion of β-endorphin and that this secretion is correlated with improved mood states.[73] Moderate intensity exercise produces the greatest increase in β-endorphin synthesis, while higher and lower intensity forms of exercise are associated with smaller increases in β-endorphin synthesis.[73] A review on β-endorphin and exercise noted that an individual's mood improves for the remainder of the day following physical exercise and that one's mood is positively correlated with overall daily physical activity level.[73]
However, humans studies showed that pharmacological blockade of endogenous endorphins does not inhibit a runner's high, while blockade of endocannabinoids may have such an effect.[80]
Anandamide
Anandamide is an endogenous cannabinoid and retrograde neurotransmitter that binds to cannabinoid receptors (primarily CB1), in turn producing euphoria.[68][74] It has been shown that aerobic exercise causes an increase in plasma anandamide levels, where the magnitude of this increase is highest at moderate exercise intensity (i.e., exercising at ~70–80% maximum heart rate).[74] Increases in plasma anandamide levels are associated with psychoactive effects because anandamide is able to cross the blood–brain barrier and act within the central nervous system.[74] Thus, because anandamide is a euphoriant and aerobic exercise is associated with euphoric effects, it has been proposed that anandamide partly mediates the short-term mood-lifting effects of exercise (e.g., the euphoria of a runner's high) via exercise-induced increases in its synthesis.[68][74]
Cortisol and the psychological stress response
.svg.png.webp)
The "stress hormone", cortisol, is a glucocorticoid that binds to glucocorticoid receptors.[81][82][83] Psychological stress induces the release of cortisol from the adrenal gland by activating the hypothalamic–pituitary–adrenal axis (HPA axis).[81][82][83] Short-term increases in cortisol levels are associated with adaptive cognitive improvements, such as enhanced inhibitory control;[82][83] however, excessively high exposure or prolonged exposure to high levels of cortisol causes impairments in cognitive control and has neurotoxic effects in the human brain.[83] For example, chronic psychological stress decreases BDNF expression, which has detrimental effects on hippocampal volume and can lead to depression.[81]
As a physical stressor, aerobic exercise stimulates cortisol secretion in an intensity-dependent manner;[82] however, it does not result in long-term increases in cortisol production since this exercise-induced effect on cortisol is a response to transient negative energy balance.[note 7][82] Aerobic exercise increases physical fitness and lowers neuroendocrine (i.e., HPA axis) reactivity and therefore reduces the biological response to psychological stress in humans (e.g., reduced cortisol release and attenuated heart rate response).[12][84] Exercise also reverses stress-induced decreases in BDNF expression and signaling in the brain, thereby acting as a buffer against stress-related diseases like depression.[81][84]
Glutamate and GABA
Glutamate, one of the most common neurochemicals in the brain, is an excitatory neurotransmitter involved in many aspects of brain function, including learning and memory.[85] Based upon animal models, exercise appears to normalize the excessive levels of glutamate neurotransmission into the nucleus accumbens that occurs in drug addiction.[21] A review of the effects of exercise on neurocardiac function in preclinical models noted that exercise-induced neuroplasticity of the rostral ventrolateral medulla (RVLM) has an inhibitory effect on glutamatergic neurotransmission in this region, in turn reducing sympathetic activity;[86] the review hypothesized that this neuroplasticity in the RVLM is a mechanism by which regular exercise prevents inactivity-related cardiovascular disease.[86]
Exerkines and other circulating compounds
Exerkines are putative "signalling moieties released in response to acute and/or chronic exercise, which exert their effects through endocrine, paracrine and/or autocrine pathways".[87]
Effects in children
Engaging in active physical pursuits has demonstrated positive effects on the mental health of children and adolescents,[88] enhances their academic performance,[89] boosts cognitive function,[90] and diminishes the likelihood of obesity and cardiovascular diseases among this demographic.[91] Establishing consistent exercise routines with regular frequency and duration is pivotal.[92][93][94] Cultivating beneficial exercise habits and sustaining adequate physical activity may support the overall physical and mental well-being of young individuals. Therefore, identifying factors that either impede or encourage exercise behaviors could be a significant strategy in promoting the development of healthy exercise habits among children and adolescents.
A 2003 meta-analysis found a positive effect of exercise in children on perceptual skills, intelligence quotient, achievement, verbal tests, mathematic tests, and academic readiness.[95] The correlation was strongest for the age ranges of 4–7 and 11–13 years.[95]
A 2010 meta-analysis of the effect of activity on children's executive function found that aerobic exercise may briefly aid children's executive function and also influence more lasting improvements to executive function.[96] Other studies suggested that exercise is unrelated to academic performance, perhaps due to the parameters used to determine exactly what academic achievement is.[97] This area of study has been a focus for education boards that make decisions on whether physical education should be implemented in the school curriculum, how much time should be dedicated to physical education, and its impact on other academic subjects.[95]
Another study found that sixth-graders who participated in vigorous physical activity at least three times a week had the highest scores compared to those who participated in moderate or no physical activity at all. Children who participated in vigorous physical activity scored three points higher, on average, on their academic test, which consisted of math, science, English, and world studies.[98]
Neuroimaging studies indicate that exercise may influence changes in brain structure and function.[97] Some investigations have linked low levels of aerobic fitness in children with impaired executive function when older as adults, but lack of selective attention, response inhibition, and interference control may also explain this outcome.[99]
Effects on central nervous system disorders
Exercise as prevention and treatment of drug addictions
Clinical and preclinical evidence indicate that consistent aerobic exercise, especially endurance exercise (e.g., marathon running), actually prevents the development of certain drug addictions and is an effective adjunct treatment for drug addiction, and psychostimulant addiction in particular.[20][21][22][23] Consistent aerobic exercise magnitude-dependently (i.e., by duration and intensity) may reduce drug addiction risk, which appears to occur through the reversal of drug-induced, addiction-related neuroplasticity.[21][22] Moreover, aerobic exercise decreases psychostimulant self-administration, reduces the reinstatement (i.e., relapse) of drug-seeking, and induces opposite effects on striatal dopamine receptor D2 (DRD2) signaling (increased DRD2 density) to those induced by pathological stimulant use (decreased DRD2 density).[21][22] Consequently, consistent aerobic exercise may lead to better treatment outcomes when used as an adjunct treatment for drug addiction.[21][23] As of 2016, more clinical research is still needed to understand the mechanisms and confirm the efficacy of exercise in drug addiction treatment and prevention.[20]
| Form of neuroplasticity or behavioral plasticity |
Type of reinforcer | Sources | |||||
|---|---|---|---|---|---|---|---|
| Opiates | Psychostimulants | High fat or sugar food | Sexual intercourse | Physical exercise (aerobic) |
Environmental enrichment | ||
| ΔFosB expression in nucleus accumbens D1-type MSNs |
↑ | ↑ | ↑ | ↑ | ↑ | ↑ | [22] |
| Behavioral plasticity | |||||||
| Escalation of intake | Yes | Yes | Yes | [22] | |||
| Psychostimulant cross-sensitization |
Yes | Not applicable | Yes | Yes | Attenuated | Attenuated | [22] |
| Psychostimulant self-administration |
↑ | ↑ | ↓ | ↓ | ↓ | [22] | |
| Psychostimulant conditioned place preference |
↑ | ↑ | ↓ | ↑ | ↓ | ↑ | [22] |
| Reinstatement of drug-seeking behavior | ↑ | ↑ | ↓ | ↓ | [22] | ||
| Neurochemical plasticity | |||||||
| CREB phosphorylation in the nucleus accumbens |
↓ | ↓ | ↓ | ↓ | ↓ | [22] | |
| Sensitized dopamine response in the nucleus accumbens |
No | Yes | No | Yes | [22] | ||
| Altered striatal dopamine signaling | ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD2 | ↑DRD2 | [22] | |
| Altered striatal opioid signaling | No change or ↑μ-opioid receptors | ↑μ-opioid receptors ↑κ-opioid receptors | ↑μ-opioid receptors | ↑μ-opioid receptors | No change | No change | [22] |
| Changes in striatal opioid peptides | ↑dynorphin No change: enkephalin | ↑dynorphin | ↓enkephalin | ↑dynorphin | ↑dynorphin | [22] | |
| Mesocorticolimbic synaptic plasticity | |||||||
| Number of dendrites in the nucleus accumbens | ↓ | ↑ | ↑ | [22] | |||
| Dendritic spine density in the nucleus accumbens |
↓ | ↑ | ↑ | [22] | |||
Attention deficit hyperactivity disorder
Regular physical exercise, particularly aerobic exercise, is an effective add-on treatment for ADHD in children and adults, particularly when combined with stimulant medication (i.e., amphetamine or methylphenidate), although the best intensity and type of aerobic exercise for improving symptoms are not currently known.[18][100] In particular, the long-term effects of regular aerobic exercise in ADHD individuals include better behavior and motor abilities, improved executive functions (including attention, inhibitory control, and planning, among other cognitive domains), faster information processing speed, and better memory.[18] Parent-teacher ratings of behavioral and socio-emotional outcomes in response to regular aerobic exercise include: better overall function, reduced ADHD symptoms, better self-esteem, reduced levels of anxiety and depression, fewer somatic complaints, better academic and classroom behavior, and improved social behavior.[18] Exercising while on stimulant medication augments the effect of stimulant medication on executive function.[18] It is believed that these short-term effects of exercise are mediated by an increased abundance of synaptic dopamine and norepinephrine in the brain.[18]
Major depressive disorder
A number of medical reviews have indicated that exercise has a marked and persistent antidepressant effect in humans,[5][16][101][17][102][103] an effect believed to be mediated through enhanced BDNF signaling in the brain.[17] Several systematic reviews have analyzed the potential for physical exercise in the treatment of depressive disorders. The 2013 Cochrane Collaboration review on physical exercise for depression noted that, based upon limited evidence, it is more effective than a control intervention and comparable to psychological or antidepressant drug therapies.[102] Three subsequent 2014 systematic reviews that included the Cochrane review in their analysis concluded with similar findings: one indicated that physical exercise is effective as an adjunct treatment (i.e., treatments that are used together) with antidepressant medication;[17] the other two indicated that physical exercise has marked antidepressant effects and recommended the inclusion of physical activity as an adjunct treatment for mild–moderate depression and mental illness in general.[16][101] One systematic review noted that yoga may be effective in alleviating symptoms of prenatal depression.[104] Another review asserted that evidence from clinical trials supports the efficacy of physical exercise as a treatment for depression over a 2–4 month period.[5] These benefits have also been noted in old age, with a review conducted in 2019 finding that exercise is an effective treatment for clinically diagnosed depression in older adults.[105]
A meta-analysis from July 2016 concluded that physical exercise improves overall quality of life in individuals with depression relative to controls.[9][106]
Cerebrovascular disease
Physical exercise plays a significant role in the prevention and management of stroke. It is well established that physical activity decrease the risk of ischemic stroke and intracerebral haemorrhage.[107][108] Engaging in physical activity before experiencing a stroke has been found to have a positive impact on the severity and outcomes of stroke.[109] Exercise has the potential to increase the expression of VEGF, caveolin, and angiopoietin in the brain. These changes may promote angiogenesis and neovascularization that contribute to improved blood supply to the stroke affected areas of the brain.[110][111][112] Exercise may affect the activation of endothelial nitric oxide synthase (eNOS) and subsequent production of nitric oxide (NO).[113][114][115] The increase in NO production may lead to improved post-stroke cerebral blood flow, ensuring a sufficient oxygen and nutrient supply to the brain. Physical activity has been associated with increased expression and activation of hypoxia-inducible factor 1 alpha (HIF-1α), heat shock proteins, and brain-derived neurotrophic factor (BDNF).[116][117][118] These factors play crucial roles in promoting cellular survival, neuroprotection, and repair processes in the brain following a stroke. Exercise also inhibit glutamate and caspase activities, which are involved in neuronal death pathways.[119][120][121][122] Additionally, it may promote neurogenesis in the brain. These effects collectively contribute to the reduction of brain infarction and edema, leading to potential improvements in neurological and functional outcomes. The neuroprotective properties of physical activity in relation to haemorrhagic strokes are less studied. Pre-stroke physical activity has been associated with improved outcomes after intracerebral haemorrhages.[123] Furthermore, physical activity may reduce the volume of intracerebral haemorrhages.[124][125] Being physically active after stroke also enhance the functional recovery.[126][127][128]
Mild cognitive impairment
The American Academy of Neurology's January 2018 update of their clinical practice guideline for mild cognitive impairment states that clinicians should recommend regular exercise (two times per week) to individuals who have been diagnosed with this condition.[19] This guidance is based upon a moderate amount of high-quality evidence which supports the efficacy of regular physical exercise (twice weekly over a 6-month period) for improving cognitive symptoms in individuals with mild cognitive impairment.[19]
Neurodegenerative disorders
Alzheimer's disease
Alzheimer's disease is a cortical neurodegenerative disorder and the most prevalent form of dementia, representing approximately 65% of all cases of dementia; it is characterized by impaired cognitive function, behavioral abnormalities, and a reduced capacity to perform basic activities of daily life.[24] Two reviews found evidence for possible positive effects of physical exercise on cognitive function, the rate of cognitive decline, and the ability to perform activities of daily living in individuals with Alzheimer's disease.[24] A subsequent review found higher levels of physical activity may be associated with reduced risk of dementia and cognitive decline.[26]
Parkinson's disease
Parkinson's disease symptoms reflect various functional impairments and limitations, such as postural instability, gait disturbance, immobility, and frequent falls. Some evidence suggests that physical exercise may lower the risk of Parkinson's disease.[129] A 2017 study found that strength and endurance training in people with Parkinson's disease had positive effects lasting for several weeks.[130]
See also
Notes
- ↑ Neurotrophic factors are peptides or other small proteins that promote the growth, survival, and differentiation of neurons by binding to and activating their associated tyrosine kinases.[28]
- ↑ Adult neurogenesis is the postnatal (after-birth) growth of new neurons, a beneficial form of neuroplasticity.[27]
- ↑ Attentional control allows an individual to focus their attention on a specific source and ignore other stimuli that compete for one's attention,[32] such as in the cocktail party effect.
- ↑ Inhibitory control is the process of altering one's learned behavioral responses, sometimes called "prepotent responses", in a way that makes it easier to complete a particular goal.[38][46] Inhibitory control allows individuals to control their impulses and habits when necessary or desired,[38][46] e.g., to overcome procrastination.
- ↑ Working memory is the form of memory used by an individual at any given moment for active information processing,[32] such as when reading or writing an encyclopedia article. Working memory has a limited capacity and functions as an information buffer, analogous to a computer's data buffer, that permits the manipulation of information for comprehension, decision-making, and guidance of behavior.[38]
- ↑ Declarative memory, also known as explicit memory, is the form of memory that pertains to facts and events.[39]
- ↑ In healthy individuals, this energy deficit resolves simply from eating and drinking a sufficient amount of food and beverage after exercising.
References
- 1 2 3 4 5 6 7 8 9 10 Erickson KI, Hillman CH, Kramer AF (August 2015). "Physical activity, brain, and cognition". Current Opinion in Behavioral Sciences. 4: 27–32. doi:10.1016/j.cobeha.2015.01.005. S2CID 54301951.
- 1 2 Paillard T, Rolland Y, de Souto Barreto P (July 2015). "Protective Effects of Physical Exercise in Alzheimer's Disease and Parkinson's Disease: A Narrative Review". J Clin Neurol. 11 (3): 212–219. doi:10.3988/jcn.2015.11.3.212. PMC 4507374. PMID 26174783.
- ↑ McKee AC, Daneshvar DH, Alvarez VE, Stein TD (January 2014). "The neuropathology of sport". Acta Neuropathol. 127 (1): 29–51. doi:10.1007/s00401-013-1230-6. PMC 4255282. PMID 24366527.
- 1 2 3 4 Denham J, Marques FZ, O'Brien BJ, Charchar FJ (February 2014). "Exercise: putting action into our epigenome". Sports Med. 44 (2): 189–209. doi:10.1007/s40279-013-0114-1. PMID 24163284. S2CID 30210091.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Gomez-Pinilla F, Hillman C (January 2013). "The influence of exercise on cognitive abilities". Comprehensive Physiology. 3 (1): 403–428. doi:10.1002/cphy.c110063. ISBN 9780470650714. PMC 3951958. PMID 23720292.
- 1 2 3 4 5 6 7 Buckley J, Cohen JD, Kramer AF, McAuley E, Mullen SP (2014). "Cognitive control in the self-regulation of physical activity and sedentary behavior". Front Hum Neurosci. 8: 747. doi:10.3389/fnhum.2014.00747. PMC 4179677. PMID 25324754.
- 1 2 3 4 5 Cox EP, O'Dwyer N, Cook R, Vetter M, Cheng HL, Rooney K, O'Connor H (August 2016). "Relationship between physical activity and cognitive function in apparently healthy young to middle-aged adults: A systematic review". J. Sci. Med. Sport. 19 (8): 616–628. doi:10.1016/j.jsams.2015.09.003. PMID 26552574.
- ↑ CDC (1 August 2023). "Benefits of Physical Activity". Centers for Disease Control and Prevention. Retrieved 7 December 2023.
- 1 2 3 Schuch FB, Vancampfort D, Rosenbaum S, Richards J, Ward PB, Stubbs B (July 2016). "Exercise improves physical and psychological quality of life in people with depression: A meta-analysis including the evaluation of control group response". Psychiatry Res. 241: 47–54. doi:10.1016/j.psychres.2016.04.054. PMID 27155287. S2CID 4787287.
- ↑ Pratali L, Mastorci F, Vitiello N, Sironi A, Gastaldelli A, Gemignani A (November 2014). "Motor Activity in Aging: An Integrated Approach for Better Quality of Life". International Scholarly Research Notices. 2014: 257248. doi:10.1155/2014/257248. PMC 4897547. PMID 27351018.
- ↑ Mandolesi L, Polverino A, Montuori S, Foti F, Ferraioli G, Sorrentino P, Sorrentino G (27 April 2018). "Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits". Frontiers in Psychology. 9: 509. doi:10.3389/fpsyg.2018.00509. PMC 5934999. PMID 29755380.
- 1 2 3 4 5 6 7 Basso JC, Suzuki WA (March 2017). "The Effects of Acute Exercise on Mood, Cognition, Neurophysiology, and Neurochemical Pathways: A Review". Brain Plasticity. 2 (2): 127–152. doi:10.3233/BPL-160040. PMC 5928534. PMID 29765853.
- ↑ "Exercise and mental health". betterhealth.vic.gov.au. Department of Health & Human Services. Retrieved 19 November 2022.
- ↑ "Exercise and Mental Health". Exercise Psychology: 93–94. 2013. doi:10.5040/9781492595502.part-002. ISBN 9781492595502.
- ↑ "10 great reasons to love aerobic exercise". Mayo Clinic. Retrieved 5 December 2023.
- 1 2 3 Josefsson T, Lindwall M, Archer T (2014). "Physical exercise intervention in depressive disorders: meta-analysis and systematic review". Scand J Med Sci Sports. 24 (2): 259–272. doi:10.1111/sms.12050. PMID 23362828. S2CID 29351791.
- 1 2 3 4 Mura G, Moro MF, Patten SB, Carta MG (2014). "Exercise as an add-on strategy for the treatment of major depressive disorder: a systematic review". CNS Spectr. 19 (6): 496–508. doi:10.1017/S1092852913000953. PMID 24589012. S2CID 32304140.
- 1 2 3 4 5 6 Den Heijer AE, Groen Y, Tucha L, Fuermaier AB, Koerts J, Lange KW, Thome J, Tucha O (July 2016). "Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review". J. Neural Transm. (Vienna). 124 (Suppl 1): 3–26. doi:10.1007/s00702-016-1593-7. PMC 5281644. PMID 27400928.
- 1 2 3 Petersen RC, Lopez O, Armstrong MJ, Getchius T, Ganguli M, Gloss D, Gronseth GS, Marson D, Pringsheim T, Day GS, Sager M, Stevens J, Rae-Grant A (January 2018). "Practice guideline update summary: Mild cognitive impairment – Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology". Neurology. Special article. 90 (3): 126–135. doi:10.1212/WNL.0000000000004826. PMC 5772157. PMID 29282327.
- 1 2 3 Carroll ME, Smethells JR (February 2016). "Sex Differences in Behavioral Dyscontrol: Role in Drug Addiction and Novel Treatments". Front. Psychiatry. 6: 175. doi:10.3389/fpsyt.2015.00175. PMC 4745113. PMID 26903885.
- 1 2 3 4 5 6 Lynch WJ, Peterson AB, Sanchez V, Abel J, Smith MA (September 2013). "Exercise as a novel treatment for drug addiction: a neurobiological and stage-dependent hypothesis". Neurosci Biobehav Rev. 37 (8): 1622–1644. doi:10.1016/j.neubiorev.2013.06.011. PMC 3788047. PMID 23806439.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Olsen CM (December 2011). "Natural rewards, neuroplasticity, and non-drug addictions". Neuropharmacology. 61 (7): 1109–1122. doi:10.1016/j.neuropharm.2011.03.010. PMC 3139704. PMID 21459101.
- 1 2 3 Linke SE, Ussher M (2015). "Exercise-based treatments for substance use disorders: evidence, theory, and practicality". Am J Drug Alcohol Abuse. 41 (1): 7–15. doi:10.3109/00952990.2014.976708. PMC 4831948. PMID 25397661.
- 1 2 3 Farina N, Rusted J, Tabet N (January 2014). "The effect of exercise interventions on cognitive outcome in Alzheimer's disease: a systematic review". Int Psychogeriatr. 26 (1): 9–18. doi:10.1017/S1041610213001385. PMID 23962667. S2CID 24936334.
- ↑ Tomlinson CL, Patel S, Meek C, Herd CP, Clarke CE, Stowe R, Shah L, Sackley CM, Deane KH, Wheatley K, Ives N (September 2013). "Physiotherapy versus placebo or no intervention in Parkinson's disease". Cochrane Database Syst Rev. 9 (9): CD002817. doi:10.1002/14651858.CD002817.pub4. PMC 7120224. PMID 24018704.
- 1 2 Blondell SJ, Hammersley-Mather R, Veerman JL (May 2014). "Does physical activity prevent cognitive decline and dementia?: A systematic review and meta-analysis of longitudinal studies". BMC Public Health. 14: 510. doi:10.1186/1471-2458-14-510. PMC 4064273. PMID 24885250.
- 1 2 Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 5, 351. ISBN 9780071481274.
- ↑ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 8:Atypical Neurotransmitters". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 199, 215. ISBN 9780071481274.
- 1 2 3 Szuhany KL, Bugatti M, Otto MW (October 2014). "A meta-analytic review of the effects of exercise on brain-derived neurotrophic factor". J Psychiatr Res. 60C: 56–64. doi:10.1016/j.jpsychires.2014.10.003. PMC 4314337. PMID 25455510.
- 1 2 3 Tarumi T, Zhang R (January 2014). "Cerebral hemodynamics of the aging brain: risk of Alzheimer disease and benefit of aerobic exercise". Front Physiol. 5: 6. doi:10.3389/fphys.2014.00006. PMC 3896879. PMID 24478719.
- 1 2 3 Batouli SH, Saba V (June 2017). "At least eighty percent of brain grey matter is modifiable by physical activity: A review study". Behavioural Brain Research. 332: 204–217. doi:10.1016/j.bbr.2017.06.002. PMID 28600001. S2CID 205895178.
- 1 2 3 Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 147–148, 154–157. ISBN 9780071481274.
- ↑ Lees C, Hopkins J (2013). "Effect of aerobic exercise on cognition, academic achievement, and psychosocial function in children: a systematic review of randomized control trials". Prev Chronic Dis. 10: E174. doi:10.5888/pcd10.130010. PMC 3809922. PMID 24157077.
- ↑ Carvalho A, Rea IM, Parimon T, Cusack BJ (2014). "Physical activity and cognitive function in individuals over 60 years of age: a systematic review". Clin Interv Aging. 9: 661–682. doi:10.2147/CIA.S55520. PMC 3990369. PMID 24748784.
- 1 2 Valkanova V, Eguia Rodriguez R, Ebmeier KP (June 2014). "Mind over matter—what do we know about neuroplasticity in adults?". Int Psychogeriatr. 26 (6): 891–909. doi:10.1017/S1041610213002482. PMID 24382194. S2CID 20765865.
- ↑ Ruscheweyh R, Willemer C, Krüger K, Duning T, Warnecke T, Sommer J, Völker K, Ho HV, Mooren F, Knecht S, Flöel A (July 2011). "Physical activity and memory functions: an interventional study". Neurobiol. Aging. 32 (7): 1304–19. doi:10.1016/j.neurobiolaging.2009.08.001. PMID 19716631. S2CID 22238883.
- 1 2 3 Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, Kim JS, Heo S, Alves H, White SM, Wojcicki TR, Mailey E, Vieira VJ, Martin SA, Pence BD, Woods JA, McAuley E, Kramer AF (February 2011). "Exercise training increases size of hippocampus and improves memory". Proc. Natl. Acad. Sci. U.S.A. 108 (7): 3017–3022. Bibcode:2011PNAS..108.3017E. doi:10.1073/pnas.1015950108. PMC 3041121. PMID 21282661.
- 1 2 3 4 5 6 7 Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 13: Higher Cognitive Function and Behavioral Control". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 313–321. ISBN 9780071481274.
- 1 2 3 Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 148, 324–328, 438. ISBN 9780071481274.
- ↑ Grimaldi G, Argyropoulos GP, Bastian A, Cortes M, Davis NJ, Edwards DJ, Ferrucci R, Fregni F, Galea JM, Hamada M, Manto M, Miall RC, Morales-Quezada L, Pope PA, Priori A, Rothwell J, Tomlinson SP, Celnik P (2014). "Cerebellar Transcranial Direct Current Stimulation (ctDCS): A Novel Approach to Understanding Cerebellar Function in Health and Disease". Neuroscientist. 22 (1): 83–97. doi:10.1177/1073858414559409. PMC 4712385. PMID 25406224.
- ↑ Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 147, 266, 376. ISBN 9780071481274.
- ↑ Sereno MI, Huang RS (2014). "Multisensory maps in parietal cortex". Curr. Opin. Neurobiol. 24 (1): 39–46. doi:10.1016/j.conb.2013.08.014. PMC 3969294. PMID 24492077.
- ↑ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 13: Higher Cognitive Function and Behavioral Control". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 315. ISBN 9780071481274.
- 1 2 3 Janssen M, Toussaint HM, van Mechelen W, Verhagen EA (2014). "Effects of acute bouts of physical activity on children's attention: a systematic review of the literature". SpringerPlus. 3: 410. doi:10.1186/2193-1801-3-410. PMC 4132441. PMID 25133092.
- ↑ Moreau D, Kirk IJ, Waldie, KE (2017). "High-intensity training enhances executive function in children in a randomized, placebo-controlled trial". eLife. 6:e25062. doi:10.7554/eLife.25062. PMC 5566451. PMID 28825973.
- 1 2 Ilieva IP, Hook CJ, Farah MJ (2015). "Prescription Stimulants' Effects on Healthy Inhibitory Control, Working Memory, and Episodic Memory: A Meta-analysis". J Cogn Neurosci. 27 (6): 1–21. doi:10.1162/jocn_a_00776. PMID 25591060. S2CID 15788121.
- ↑ Northey JM, Cherbuin N, Pumpa KL, Smee DJ, Rattray B (February 2018). "Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis". British Journal of Sports Medicine. 52 (3): 154–160. doi:10.1136/bjsports-2016-096587. PMID 28438770. S2CID 13553374.
- ↑ Delezie J, Handschin C (24 August 2018). "Endocrine Crosstalk Between Skeletal Muscle and the Brain". Frontiers in Neurology. 9: 698. doi:10.3389/fneur.2018.00698. PMC 6117390. PMID 30197620.
- ↑ Kim S, Choi JY, Moon S, Park DH, Kwak HB, Kang JH (March 2019). "Roles of myokines in exercise-induced improvement of neuropsychiatric function". Pflügers Archiv. 471 (3): 491–505. doi:10.1007/s00424-019-02253-8. PMID 30627775. S2CID 57765282.
- 1 2 3 4 5 6 7 Phillips C, Baktir MA, Srivatsan M, Salehi A (2014). "Neuroprotective effects of physical activity on the brain: a closer look at trophic factor signaling". Front Cell Neurosci. 8: 170. doi:10.3389/fncel.2014.00170. PMC 4064707. PMID 24999318.
- 1 2 3 Heinonen I, Kalliokoski KK, Hannukainen JC, Duncker DJ, Nuutila P, Knuuti J (November 2014). "Organ-Specific Physiological Responses to Acute Physical Exercise and Long-Term Training in Humans". Physiology. 29 (6): 421–436. doi:10.1152/physiol.00067.2013. PMID 25362636.
- ↑ Anderson E, Shivakumar G (2013). "Effects of exercise and physical activity on anxiety". Frontiers in Psychiatry. 4: 27. doi:10.3389/fpsyt.2013.00027. PMC 3632802. PMID 23630504.
- 1 2 3 4 Torres-Aleman I (2010). "Toward a comprehensive neurobiology of IGF-I". Dev Neurobiol. 70 (5): 384–96. doi:10.1002/dneu.20778. PMID 20186710. S2CID 27947753.
- 1 2 3 Aberg D (2010). "Role of the growth hormone/insulin-like growth factor 1 axis in neurogenesis". Endocr Dev. Endocrine Development. 17: 63–76. doi:10.1159/000262529. ISBN 978-3-8055-9302-1. PMID 19955757.
- 1 2 3 Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 221, 412. ISBN 9780071481274.
- ↑ Gatti R, De Palo EF, Antonelli G, Spinella P (July 2012). "IGF-I/IGFBP system: metabolism outline and physical exercise". J. Endocrinol. Invest. 35 (7): 699–707. doi:10.3275/8456. PMID 22714057. S2CID 22974661.
- 1 2 Bouchard J, Villeda SA (2015). "Aging and brain rejuvenation as systemic events". J. Neurochem. 132 (1): 5–19. doi:10.1111/jnc.12969. PMC 4301186. PMID 25327899.
- ↑ "The hormone irisin is found to confer benefits of exercise on cognitive function". medicalxpress.com. Retrieved 21 September 2021.
- ↑ Reynolds G (25 August 2021). "How Exercise May Help Keep Our Memory Sharp". The New York Times. Retrieved 21 September 2021.
- ↑ Islam MR, Valaris S, Young MF, Haley EB, Luo R, Bond SF, et al. (August 2021). "Exercise hormone irisin is a critical regulator of cognitive function". Nature Metabolism. 3 (8): 1058–1070. doi:10.1038/s42255-021-00438-z. PMC 10317538. PMID 34417591. S2CID 237254736.
- ↑ Maak S, Norheim F, Drevon CA, Erickson HP (July 2021). "Progress and Challenges in the Biology of FNDC5 and Irisin". Endocrine Reviews. 42 (4): 436–456. doi:10.1210/endrev/bnab003. PMC 8284618. PMID 33493316.
- 1 2 Basso JC, Shang A, Elman M, Karmouta R, Suzuki WA (November 2015). "Acute Exercise Improves Prefrontal Cortex but not Hippocampal Function in Healthy Adults". Journal of the International Neuropsychological Society. 21 (10): 791–801. doi:10.1017/S135561771500106X. PMID 26581791.
- 1 2 McMorris T, Hale BJ (December 2012). "Differential effects of differing intensities of acute exercise on speed and accuracy of cognition: a meta-analytical investigation". Brain and Cognition. 80 (3): 338–351. doi:10.1016/j.bandc.2012.09.001. PMID 23064033. S2CID 8320775.
- ↑ Dodwell G, Müller HJ, Töllner T (May 2019). "Electroencephalographic evidence for improved visual working memory performance during standing and exercise". British Journal of Psychology. 110 (2): 400–427. doi:10.1111/bjop.12352. PMID 30311188. S2CID 52960179.
- ↑ Dodwell G, Liesefeld HR, Conci M, Müller HJ, Töllner T (December 2021). "EEG evidence for enhanced attentional performance during moderate-intensity exercise". Psychophysiology. 58 (12): e13923. doi:10.1111/psyp.13923. ISSN 0048-5772. PMID 34370887. S2CID 236969156.
- ↑ Cunha GS, Ribeiro JL, Oliveira AR (June 2008). "[Levels of beta-endorphin in response to exercise and overtraining]". Arq Bras Endocrinol Metabol (in Portuguese). 52 (4): 589–598. doi:10.1590/S0004-27302008000400004. hdl:10183/40053. PMID 18604371.
- ↑ Boecker H, Sprenger T, Spilker ME, Henriksen G, Koppenhoefer M, Wagner KJ, Valet M, Berthele A, Tolle TR (2008). "The runner's high: opioidergic mechanisms in the human brain". Cereb. Cortex. 18 (11): 2523–2531. doi:10.1093/cercor/bhn013. PMID 18296435.
The runner's high describes an euphoric state resulting from long-distance running.
- 1 2 3 Raichlen DA, Foster AD, Gerdeman GL, Seillier A, Giuffrida A (2012). "Wired to run: exercise-induced endocannabinoid signaling in humans and cursorial mammals with implications for the 'runner's high'". J. Exp. Biol. 215 (Pt 8): 1331–1336. doi:10.1242/jeb.063677. PMID 22442371. S2CID 5129200.
- ↑ Cohen EE, Ejsmond-Frey R, Knight N, Dunbar RI (2010). "Rowers' high: behavioural synchrony is correlated with elevated pain thresholds". Biol. Lett. 6 (1): 106–108. doi:10.1098/rsbl.2009.0670. PMC 2817271. PMID 19755532.
- 1 2 3 4 5 Szabo A, Billett E, Turner J (2001). "Phenylethylamine, a possible link to the antidepressant effects of exercise?". Br J Sports Med. 35 (5): 342–343. doi:10.1136/bjsm.35.5.342. PMC 1724404. PMID 11579070.
- 1 2 3 4 5 Lindemann L, Hoener MC (2005). "A renaissance in trace amines inspired by a novel GPCR family". Trends Pharmacol. Sci. 26 (5): 274–281. doi:10.1016/j.tips.2005.03.007. PMID 15860375.
- 1 2 3 4 5 Berry MD (2007). "The potential of trace amines and their receptors for treating neurological and psychiatric diseases". Rev Recent Clin Trials. 2 (1): 3–19. CiteSeerX 10.1.1.329.563. doi:10.2174/157488707779318107. PMID 18473983.
- 1 2 3 4 5 Dinas PC, Koutedakis Y, Flouris AD (2011). "Effects of exercise and physical activity on depression". Ir J Med Sci. 180 (2): 319–325. doi:10.1007/s11845-010-0633-9. PMID 21076975. S2CID 40951545.
- 1 2 3 4 5 Tantimonaco M, Ceci R, Sabatini S, Catani MV, Rossi A, Gasperi V, Maccarrone M (2014). "Physical activity and the endocannabinoid system: an overview". Cell. Mol. Life Sci. 71 (14): 2681–2698. doi:10.1007/s00018-014-1575-6. PMID 24526057. S2CID 14531019.
- ↑ Broadley KJ (March 2010). "The vascular effects of trace amines and amphetamines". Pharmacology & Therapeutics. 125 (3): 363–375. doi:10.1016/j.pharmthera.2009.11.005. PMID 19948186.
- ↑ Lindemann L, Hoener MC (May 2005). "A renaissance in trace amines inspired by a novel GPCR family". Trends in Pharmacological Sciences. 26 (5): 274–281. doi:10.1016/j.tips.2005.03.007. PMID 15860375.
- ↑ Wang X, Li J, Dong G, Yue J (February 2014). "The endogenous substrates of brain CYP2D". European Journal of Pharmacology. 724: 211–218. doi:10.1016/j.ejphar.2013.12.025. PMID 24374199.
- ↑ Berry MD, Gainetdinov RR, Hoener MC, Shahid M (December 2017). "Pharmacology of human trace amine-associated receptors: Therapeutic opportunities and challenges". Pharmacology & Therapeutics. 180: 161–180. doi:10.1016/j.pharmthera.2017.07.002. PMID 28723415. S2CID 207366162.
- 1 2 Broadley KJ (March 2010). "The vascular effects of trace amines and amphetamines". Pharmacol. Ther. 125 (3): 363–375. doi:10.1016/j.pharmthera.2009.11.005. PMID 19948186.
- ↑ Siebers M, Biedermann SV, Bindila L, Lutz B, Fuss J (April 2021). "Exercise-induced euphoria and anxiolysis do not depend on endogenous opioids in humans". Psychoneuroendocrinology. 126: 105173. doi:10.1016/j.psyneuen.2021.105173. PMID 33582575. S2CID 231858251.
- 1 2 3 4 Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 14: Mood and Emotion". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 350–359. ISBN 9780071481274.
- 1 2 3 4 5 Fuqua JS, Rogol AD (July 2013). "Neuroendocrine alterations in the exercising human: implications for energy homeostasis". Metab. Clin. Exp. 62 (7): 911–921. doi:10.1016/j.metabol.2013.01.016. PMID 23415825.
- 1 2 3 4 Ebner NC, Kamin H, Diaz V, Cohen RA, MacDonald K (January 2015). "Hormones as 'difference makers' in cognitive and socioemotional aging processes". Front Psychol. 5: 1595. doi:10.3389/fpsyg.2014.01595. PMC 4302708. PMID 25657633.
- 1 2 Zschucke E, Gaudlitz K, Ströhle A (January 2013). "Exercise and physical activity in mental disorders: clinical and experimental evidence". J Prev Med Public Health. 46 (Suppl 1): S12–521. doi:10.3961/jpmph.2013.46.S.S12. PMC 3567313. PMID 23412549.
- ↑ Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 5: Excitatory and Inhibitory Amino Acids". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 117–130. ISBN 9780071481274.
- 1 2 Mischel NA, Subramanian M, Dombrowski MD, Llewellyn-Smith IJ, Mueller PJ (May 2015). "(In)activity-related neuroplasticity in brainstem control of sympathetic outflow: unraveling underlying molecular, cellular, and anatomical mechanisms". Am. J. Physiol. Heart Circ. Physiol. 309 (2): H235–43. doi:10.1152/ajpheart.00929.2014. PMC 4504968. PMID 25957223.
- ↑ Chow LS, Gerszten RE, Taylor JM, et al. (May 2022). "Exerkines in health, resilience and disease". Nature Reviews. Endocrinology. 18 (5): 273–289. doi:10.1038/s41574-022-00641-2. PMC 9554896. PMID 35304603.
- ↑ Strong WB, Malina RM, Blimkie CJ, et al. (June 2005). "Evidence Based Physical Activity for School-age Youth". The Journal of Pediatrics. 146 (6): 732–737. doi:10.1016/j.jpeds.2005.01.055. ISSN 0022-3476. PMID 15973308.
- ↑ "Physical activity levels among children aged 9-13 years: United States, 2002". PsycEXTRA Dataset. 2002. doi:10.1037/e303072004-001. Retrieved 8 December 2023.
- ↑ Ebbeling CB, Pawlak DB, Ludwig DS (August 2002). "Childhood obesity: public-health crisis, common sense cure". The Lancet. 360 (9331): 473–482. doi:10.1016/s0140-6736(02)09678-2. ISSN 0140-6736. PMID 12241736. S2CID 6374501.
- ↑ Ward DS, Saunders RP, Pate RR (2007). Physical Activity Interventions in Children and Adolescents. doi:10.5040/9781492596868. ISBN 9781492596868.
- ↑ van Sluijs EM, McMinn AM, Griffin SJ (20 September 2007). "Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials". BMJ. 335 (7622): 703. doi:10.1136/bmj.39320.843947.be. ISSN 0959-8138. PMC 2001088. PMID 17884863. S2CID 5659723.
- ↑ Pate RR, Trost SG, Mullis R, Sallis JF, Wechsler H, Brown DR (August 2000). "Community Interventions to Promote Proper Nutrition and Physical Activity among Youth". Preventive Medicine. 31 (2): S138–S149. doi:10.1006/pmed.2000.0632. ISSN 0091-7435.
- ↑ Stone EJ, McKenzie TL, Welk GJ, Booth ML (November 1998). "Effects of physical activity interventions in youth". American Journal of Preventive Medicine. 15 (4): 298–315. doi:10.1016/s0749-3797(98)00082-8. ISSN 0749-3797. PMID 9838974.
- 1 2 3 Sibley BA, Etnier JL (August 2003). "The Relationship between Physical Activity and Cognition in Children: A Meta-Analysis". Pediatric Exercise Science. 15 (3): 243–256. doi:10.1123/pes.15.3.243. S2CID 56815489.
- ↑ Best JR (December 2010). "Effects of Physical Activity on Children's Executive Function: Contributions of Experimental Research on Aerobic Exercise". Developmental Review. 30 (4): 331–551. doi:10.1016/j.dr.2010.08.001. PMC 3147174. PMID 21818169.
- 1 2 Hillman CH, Erickson KI, Kramer AF (January 2008). "Be smart, exercise your heart: exercise effects on brain and cognition". Nature Reviews. Neuroscience. 9 (1): 58–65. doi:10.1038/nrn2298. PMID 18094706. S2CID 1204039.
- ↑ Coe DP, Pivarnik JM, Womack CJ, Reeves MJ, Malina RM (August 2006). "Effect of physical education and activity levels on academic achievement in children". Medicine and Science in Sports and Exercise. 38 (8): 1515–1519. doi:10.1249/01.mss.0000227537.13175.1b. PMID 16888468. S2CID 9676116.
- ↑ Chaddock L, Hillman CH, Buck SM, Cohen NJ (February 2011). "Aerobic fitness and executive control of relational memory in preadolescent children". Medicine and Science in Sports and Exercise. 43 (2): 344–349. doi:10.1249/MSS.0b013e3181e9af48. PMID 20508533. S2CID 400283.
- ↑ Rommel AS, Halperin JM, Mill J, Asherson P, Kuntsi J (September 2013). "Protection from genetic diathesis in attention-deficit/hyperactivity disorder: possible complementary roles of exercise". J. Am. Acad. Child Adolesc. Psychiatry. 52 (9): 900–910. doi:10.1016/j.jaac.2013.05.018. PMC 4257065. PMID 23972692.
- 1 2 Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB (2014). "Physical activity interventions for people with mental illness: a systematic review and meta-analysis". J Clin Psychiatry. 75 (9): 964–974. doi:10.4088/JCP.13r08765. PMID 24813261.
- 1 2 Cooney GM, Dwan K, Greig CA, Lawlor DA, Rimer J, Waugh FR, McMurdo M, Mead GE (September 2013). "Exercise for depression". Cochrane Database Syst. Rev. 2013 (9): CD004366. doi:10.1002/14651858.CD004366.pub6. PMC 9721454. PMID 24026850.
- ↑ Brené S, Bjørnebekk A, Aberg E, Mathé AA, Olson L, Werme M (2007). "Running is rewarding and antidepressive". Physiol. Behav. 92 (1–2): 136–140. doi:10.1016/j.physbeh.2007.05.015. PMC 2040025. PMID 17561174.
- ↑ Gong H, Ni C, Shen X, Wu T, Jiang C (February 2015). "Yoga for prenatal depression: a systematic review and meta-analysis". BMC Psychiatry. 15: 14. doi:10.1186/s12888-015-0393-1. PMC 4323231. PMID 25652267.
- ↑ Miller KJ, Gonçalves-Bradley DC, Areerob P, Hennessy D, Mesagno C, Grace F (2020). "Comparative effectiveness of three exercise types to treat clinical depression in older adults: A systematic review and network meta-analysis of randomised controlled trials". Ageing Research Reviews. 58: 100999. doi:10.1016/j.arr.2019.100999. hdl:1959.17/172086. PMID 31837462. S2CID 209179889.
- ↑ Chaturvedi SK, Chandra PS, Issac MK, Sudarshan CY (September 1993). "Somatization misattributed to non-pathological vaginal discharge". Journal of Psychosomatic Research. 37 (6): 575–579. doi:10.1016/0022-3999(93)90051-G. PMID 8410743.
- ↑ O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. (July 2010). "Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study". Lancet. 376 (9735): 112–123. doi:10.1016/s0140-6736(10)60834-3. PMID 20561675. S2CID 2753073.
- ↑ Lee CD, Folsom AR, Blair SN (October 2003). "Physical activity and stroke risk: a meta-analysis". Stroke. 34 (10): 2475–2481. doi:10.1161/01.STR.0000091843.02517.9D. PMID 14500932. S2CID 2332015.
- ↑ Viktorisson A, Reinholdsson M, Danielsson A, Palstam A, Sunnerhagen KS (January 2022). "Pre-stroke physical activity in relation to post-stroke outcomes - linked to the International Classification of Functioning, Disability and Health (ICF): A scoping review". Journal of Rehabilitation Medicine. 54: jrm00251. doi:10.2340/jrm.v53.51. PMC 8862654. PMID 34904691.
- ↑ Ding YH, Luan XD, Li J, Rafols JA, Guthinkonda M, Diaz FG, Ding Y (December 2004). "Exercise-induced overexpression of angiogenic factors and reduction of ischemia/reperfusion injury in stroke". Current Neurovascular Research. 1 (5): 411–420. doi:10.2174/1567202043361875. PMID 16181089. S2CID 22015361.
- ↑ Rezaei R, Nasoohi S, Haghparast A, Khodagholi F, Bigdeli MR, Nourshahi M (August 2018). "High intensity exercise preconditioning provides differential protection against brain injury following experimental stroke". Life Sciences. 207: 30–35. doi:10.1016/j.lfs.2018.03.007. PMID 29522768. S2CID 3812671.
- ↑ Gao Y, Zhao Y, Pan J, Yang L, Huang T, Feng X, et al. (October 2014). "Treadmill exercise promotes angiogenesis in the ischemic penumbra of rat brains through caveolin-1/VEGF signaling pathways". Brain Research. 1585: 83–90. doi:10.1016/j.brainres.2014.08.032. PMID 25148708. S2CID 25507984.
- ↑ Endres M, Gertz K, Lindauer U, Katchanov J, Schultze J, Schröck H, et al. (November 2003). "Mechanisms of stroke protection by physical activity". Annals of Neurology. 54 (5): 582–590. doi:10.1002/ana.10722. PMID 14595647. S2CID 28445967.
- ↑ Gertz K, Priller J, Kronenberg G, Fink KB, Winter B, Schröck H, et al. (November 2006). "Physical activity improves long-term stroke outcome via endothelial nitric oxide synthase-dependent augmentation of neovascularization and cerebral blood flow". Circulation Research. 99 (10): 1132–1140. doi:10.1161/01.RES.0000250175.14861.77. PMID 17038638. S2CID 9063866.
- ↑ Hafez S, Khan MB, Awad ME, Wagner JD, Hess DC (August 2020). "Short-Term Acute Exercise Preconditioning Reduces Neurovascular Injury After Stroke Through Induced eNOS Activation". Translational Stroke Research. 11 (4): 851–860. doi:10.1007/s12975-019-00767-y. PMID 31858409. S2CID 255954922.
- ↑ Sharp FR, Bernaudin M (June 2004). "HIF1 and oxygen sensing in the brain". Nature Reviews. Neuroscience. 5 (6): 437–448. doi:10.1038/nrn1408. PMID 15152194. S2CID 318020.
- ↑ Dornbos D, Ding Y (February 2012). "Mechanisms of neuronal damage and neuroprotection underlying ischemia/reperfusion injury after physical exercise". Current Drug Targets. 13 (2): 247–262. doi:10.2174/138945012799201658. PMID 22204323.
- ↑ Wang L, Deng W, Yuan Q, Yang H (March 2015). "Exercise preconditioning reduces ischemia reperfusion-induced focal cerebral infarct volume through up-regulating the expression of HIF-1α". Pakistan Journal of Pharmaceutical Sciences. 28 (2 Suppl): 791–798. PMID 25796156.
- ↑ Jia J, Hu YS, Wu Y, Liu G, Yu HX, Zheng QP, et al. (April 2009). "Pre-ischemic treadmill training affects glutamate and gamma aminobutyric acid levels in the striatal dialysate of a rat model of cerebral ischemia". Life Sciences. 84 (15–16): 505–511. doi:10.1016/j.lfs.2009.01.015. PMID 19302809.
- ↑ Zhang F, Wu Y, Jia J, Hu YS (August 2010). "Pre-ischemic treadmill training induces tolerance to brain ischemia: involvement of glutamate and ERK1/2". Molecules. 15 (8): 5246–5257. doi:10.3390/molecules15085246. PMC 6257775. PMID 20714296.
- ↑ Yang X, He Z, Zhang Q, Wu Y, Hu Y, Wang X, et al. (26 July 2012). "Pre-ischemic treadmill training for prevention of ischemic brain injury via regulation of glutamate and its transporter GLT-1". International Journal of Molecular Sciences. 13 (8): 9447–9459. doi:10.3390/ijms13089447. PMC 3431805. PMID 22949807.
- ↑ Aboutaleb N, Shamsaei N, Khaksari M, Erfani S, Rajabi H, Nikbakht F (September 2015). "Pre-ischemic exercise reduces apoptosis in hippocampal CA3 cells after cerebral ischemia by modulation of the Bax/Bcl-2 proteins ratio and prevention of caspase-3 activation". The Journal of Physiological Sciences. 65 (5): 435–443. doi:10.1007/s12576-015-0382-7. PMC 10717499. PMID 26012958. S2CID 255606303.
- ↑ Viktorisson A, Buvarp D, Reinholdsson M, Danielsson A, Palstam A, Stibrant Sunnerhagen K (November 2022). "Associations of Prestroke Physical Activity With Stroke Severity and Mortality After Intracerebral Hemorrhage Compared With Ischemic Stroke". Neurology. 99 (19): e2137–e2148. doi:10.1212/WNL.0000000000201097. PMC 9651453. PMID 36344278.
- ↑ Viktorisson A, Buvarp D, Danielsson A, Skoglund T, Sunnerhagen KS (May 2023). "Prestroke physical activity is associated with admission haematoma volume and the clinical outcome of intracerebral haemorrhage". Stroke and Vascular Neurology. 8 (6): 511–520. doi:10.1136/svn-2023-002316. PMID 37137521. S2CID 258464205.
- ↑ Kinoshita K, Hamanaka G, Ohtomo R, Takase H, Chung KK, Lok J, et al. (May 2021). "Mature Adult Mice With Exercise-Preconditioning Show Better Recovery After Intracerebral Hemorrhage". Stroke. 52 (5): 1861–1865. doi:10.1161/STROKEAHA.120.032201. PMC 8085050. PMID 33840224.
- ↑ McKevitt C, Fudge N, Redfern J, Sheldenkar A, Crichton S, Rudd AR, et al. (May 2011). "Self-reported long-term needs after stroke". Stroke. 42 (5): 1398–1403. doi:10.1161/STROKEAHA.110.598839. PMID 21441153. S2CID 33967186.
- ↑ Buvarp D, Viktorisson A, Axelsson F, Lehto E, Lindgren L, Lundström E, Sunnerhagen KS (May 2023). "Physical Activity Trajectories and Functional Recovery After Acute Stroke Among Adults in Sweden". JAMA Network Open. 6 (5): e2310919. doi:10.1001/jamanetworkopen.2023.10919. PMC 10152305. PMID 37126346.
- ↑ Gunnes M, Indredavik B, Langhammer B, Lydersen S, Ihle-Hansen H, Dahl AE, Askim T (December 2019). "Associations Between Adherence to the Physical Activity and Exercise Program Applied in the LAST Study and Functional Recovery After Stroke". Archives of Physical Medicine and Rehabilitation. 100 (12): 2251–2259. doi:10.1016/j.apmr.2019.04.023. hdl:10642/8488. PMID 31374191. S2CID 199388335.
- ↑ Fang X, Han D, Cheng Q, Zhang P, Zhao C, Min J, Wang F (September 2018). "Association of Levels of Physical Activity With Risk of Parkinson Disease: A Systematic Review and Meta-analysis". JAMA Network Open. 1 (5): e182421. doi:10.1001/jamanetworkopen.2018.2421. PMC 6324511. PMID 30646166.
- ↑ Mak MK, Wong-Yu IS, Shen X, Chung CL (November 2017). "Long-term effects of exercise and physical therapy in people with Parkinson disease". Nature Reviews Neurology. 13 (11): 689–703. doi:10.1038/nrneurol.2017.128. ISSN 1759-4766. PMID 29027544. S2CID 29666456.