| Breast cancer | |
|---|---|
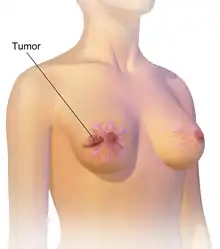 | |
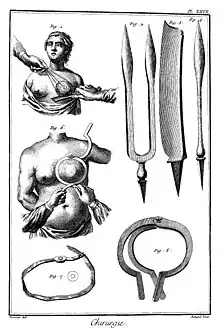
| An illustration of breast cancer | |
| Specialty | Oncology |
| Symptoms | A lump in a breast, a change in breast shape, dimpling of the skin, fluid from the nipple, a newly inverted nipple, a red scaly patch of skin on the breast[1] |
| Risk factors | Being female, obesity, lack of exercise, alcohol, hormone replacement therapy during menopause, ionizing radiation, early age at first menstruation, having children late in life or not at all, older age, prior breast cancer, family history of breast cancer, Klinefelter syndrome[1][2][3] |
| Diagnostic method | Tissue biopsy[1] Mammography |
| Treatment | Surgery, radiation therapy, chemotherapy, hormonal therapy, targeted therapy[1] |
| Prognosis | Five-year survival rate ≈85% (US, UK)[4][5] |
| Frequency | 2.2 million affected (global, 2020)[6] |
| Deaths | 685,000 (global, 2020)[6] |
Breast cancer is a cancer that develops from breast tissue.[7] Signs of breast cancer may include a lump in the breast, a change in breast shape, dimpling of the skin, milk rejection, fluid coming from the nipple, a newly inverted nipple, or a red or scaly patch of skin.[1] In those with distant spread of the disease, there may be bone pain, swollen lymph nodes, shortness of breath, or yellow skin.[8]
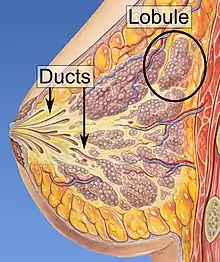
Risk factors for developing breast cancer include obesity, a lack of physical exercise, alcohol consumption, hormone replacement therapy during menopause, ionizing radiation, an early age at first menstruation, having children late in life or not at all, older age, having a prior history of breast cancer, and a family history of breast cancer.[1][2][9] About 5–10% of cases are the result of an inherited genetic predisposition,[1] including BRCA mutations among others.[1] Breast cancer most commonly develops in cells from the lining of milk ducts and the lobules that supply these ducts with milk.[1] Cancers developing from the ducts are known as ductal carcinomas, while those developing from lobules are known as lobular carcinomas.[1] There are more than 18 other sub-types of breast cancer.[2] Some, such as ductal carcinoma in situ, develop from pre-invasive lesions.[2] The diagnosis of breast cancer is confirmed by taking a biopsy of the concerning tissue.[1] Once the diagnosis is made, further tests are done to determine if the cancer has spread beyond the breast and which treatments are most likely to be effective.[1]
The balance of benefits versus harms of breast cancer screening is controversial. A 2013 Cochrane review found that it was unclear if mammographic screening does more harm than good, in that a large proportion of women who test positive turn out not to have the disease.[10] A 2009 review for the US Preventive Services Task Force found evidence of benefit in those 40 to 70 years of age,[11] and the organization recommends screening every two years in women 50 to 74 years of age.[12] The medications tamoxifen or raloxifene may be used in an effort to prevent breast cancer in those who are at high risk of developing it.[2] Surgical removal of both breasts is another preventive measure in some high risk women.[2] In those who have been diagnosed with cancer, a number of treatments may be used, including surgery, radiation therapy, chemotherapy, hormonal therapy, and targeted therapy.[1] Types of surgery vary from breast-conserving surgery to mastectomy.[13][14] Breast reconstruction may take place at the time of surgery or at a later date.[14] In those in whom the cancer has spread to other parts of the body, treatments are mostly aimed at improving quality of life and comfort.[14]
Outcomes for breast cancer vary depending on the cancer type, the extent of disease, and the person's age.[14] The five-year survival rates in England and the United States are between 80 and 90%.[15][4][5] In developing countries, five-year survival rates are lower.[2] Worldwide, breast cancer is the leading type of cancer in women, accounting for 25% of all cases.[16] In 2018, it resulted in 2 million new cases and 627,000 deaths.[17] It is more common in developed countries[2] and is more than 100 times more common in women than in men.[15][18]
Signs and symptoms

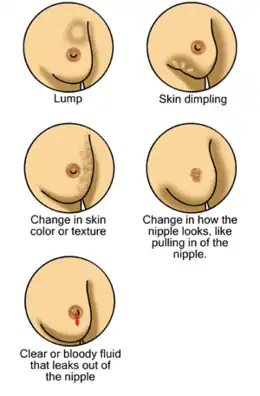
Most people with breast cancer have no symptoms at the time of diagnosis; their tumor is detected by a breast cancer screening test.[19] Those who do have symptosm commonly feel a lump that feels different from the rest of the breast tissue. Lumps found in lymph nodes located in the armpits[20] may also indicate breast cancer. Indications of breast cancer other than a lump may include thickening different from the other breast tissue, one breast becoming larger or lower, a nipple changing position or shape or becoming inverted, skin puckering or dimpling, a rash on or around a nipple, discharge from nipple/s, constant pain in part of the breast or armpit and swelling beneath the armpit or around the collarbone.[21] Pain ("mastodynia") is an unreliable tool in determining the presence or absence of breast cancer, but may be indicative of other breast health issues.[20][22][23]
Another symptom complex of breast cancer is Paget's disease of the breast. This syndrome presents as skin changes resembling eczema; such as redness, discoloration or mild flaking of the nipple skin. As Paget's disease of the breast advances, symptoms may include tingling, itching, increased sensitivity, burning, and pain. There may also be discharge from the nipple. Approximately half the women diagnosed with Paget's disease of the breast also have a lump in the breast.[24][25]
Inflammatory breast cancer is a rare (only seen in less than 5% of breast cancer diagnosis) yet aggressive form of breast cancer characterized by the swollen, red areas formed on the top of the breast. The visual effects of inflammatory breast cancer is a result of a blockage of lymph vessels by cancer cells. This type of breast cancer is seen in more commonly diagnosed in younger ages, obese women and African American women. As inflammatory breast cancer does not present as a lump there can sometimes be a delay in diagnosis.[26]
Mammary secretory carcinoma (MSC) is a rare form of the secretory carcinomas that occurs exclusively in the breast.[27] It usually develops in adults but in a significant percentage of cases also affects children:[28] MSC accounts for 80% of all childhood breast cancers.[29] MSC lesions are typically slow growing, painless, small ductal breast tumours that have invaded the tissue around their ducts of origin, often spread to sentinel lymph nodes and/or axillary lymph nodes, but rarely metastasized to distant tissues.[30] These tumours typically have distinctive microscopic features and tumour cells that carry a balanced genetic translocation in which part of the NTRK3 gene is fused to part of the ETV6 gene[31] to form a fusion gene, ETV6-NTRK3. This fusion gene encodes a chimeric protein termed ETV6-NTRK3. The NTRK3 part of ETV6-NTRK3 protein has up-regulated tyrosine kinase activity that stimulates two signaling pathways, the PI3K/AKT/mTOR and MAPK/ERK pathways, which promote cell proliferation and survival and thereby may contribute to the development of MSC.[28] Conservative surgery, modified radical mastectomy, and radical mastectomy have been the most frequent procedures used to treat adults, while simple mastectomy, local excision with sentinel lymph node biopsy, and complete axillary dissection have been recommended to treat children with MSC.[32] In all cases, long-term, e.g. >20 years, follow-up examinations are recommended.[27][31] The relatively rare cases of MSC that have metastasized to distant tissues have shown little or no responses to chemotherapy and radiotherapy. Three patients with metastatic disease had good partial responses to Entrectinib, a drug that inhibits the tyrosine kinase activity of the ETV6-NTRK3 fusion protein.[33] Because of its slow growth and low rate of metastasis to distant tissues, individuals with MSC have had 20 year survival rates of 93.16%.[27]
In rare cases, what initially appears as a fibroadenoma (hard, movable non-cancerous lump) could in fact be a phyllodes tumour. Phyllodes tumours are formed within the stroma (connective tissue) of the breast and contain glandular as well as stromal tissue. Phyllodes tumours are not staged in the usual sense; they are classified on the basis of their appearance under the microscope as benign, borderline or malignant.[34]
Malignant tumours can result in metastatic tumours – secondary tumours (originating from the primary tumour) that spread beyond the site of origination. The symptoms caused by metastatic breast cancer will depend on the location of metastasis. Common sites of metastasis include bone, liver, lung, and brain.[35] When cancer has reached such an invasive state, it is categorized as a stage 4 cancer, cancers of this state are often fatal.[36] Common symptoms of stage 4 cancer include unexplained weight loss, bone and joint pain, jaundice and neurological symptoms. These symptoms are called non-specific symptoms because they could be manifestations of many other illnesses.[37] Rarely breast cancer can spread to exceedingly uncommon sites such as peripancreatic lymph nodes causing biliary obstruction leading to diagnostic difficulties.[38]

Most symptoms of breast disorders, including most lumps, do not turn out to represent underlying breast cancer. Less than 20% of lumps, for example, are cancerous,[39] and benign breast diseases such as mastitis and fibroadenoma of the breast are more common causes of breast disorder symptoms.[40]
Risk factors
Risk factors can be divided into two categories:
- modifiable risk factors (things that people can change themselves, such as consumption of alcoholic beverages), and
- fixed risk factors (things that cannot be changed, such as age and biological sex).[41]
The primary risk factors for breast cancer are being female and older age.[42] Most breast cancers develop in women over 50. Women in their early 50s are twice as more likely to develop breast cancer than women in their early 40s.[43]
Other potential risk factors include genetics,[44] lack of childbearing or lack of breastfeeding,[45] higher levels of certain hormones,[46][47] certain dietary patterns, and obesity. Exposure to artificial light during sleeping might also be risk factor for the development of breast cancer.[48]
Actions to prevent breast cancer include not drinking alcoholic beverages, maintaining a healthy body composition, avoiding smoking and eating healthy food. Combining all of these (leading the healthiest possible lifestyle) would make almost a quarter of breast cancer cases worldwide preventable.[49] The remaining three-quarters of breast cancer cases cannot be prevented through lifestyle changes.[49]
Lifestyle
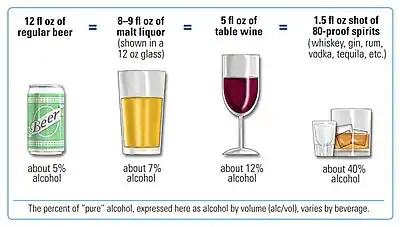
Drinking alcoholic beverages increases the risk of breast cancer, even among very light drinkers (women drinking less than half of one alcoholic drink per day).[50] The risk is highest among heavy drinkers.[52] Globally, about one in 10 cases of breast cancer is caused by women drinking alcoholic beverages.[52] Drinking alcoholic beverages is among the most common modifiable risk factors.[53]
Obesity and diabetes increase the risk of breast cancer. A high body mass index (BMI) causes 7% of breast cancers while diabetes is responsible for 2%.[43][54] At the same time the correlation between obesity and breast cancer is anything but linear. Studies show that those who rapidly gain weight in adulthood are at higher risk than those who have been overweight since childhood. Likewise excess fat in the midsection seems to induce a higher risk than excess weight carried in the lower body.[55] Dietary factors that may increase risk include a high-fat diet[56] and obesity-related high cholesterol levels.[57][58]
Dietary iodine deficiency may also play a role in the development of breast cancer.[59]
Smoking tobacco appears to increase the risk of breast cancer, with the greater the amount smoked and the earlier in life that smoking began, the higher the risk.[60] In those who are long-term smokers, the relative risk is increased 35% to 50%.[60]
A lack of physical activity has been linked to about 10% of cases.[61] Sitting regularly for prolonged periods is associated with higher mortality from breast cancer. The risk is not negated by regular exercise, though it is lowered.[62]
Breast feeding reduces the risk of several types of cancers, including breast cancer.[63][64][65][66] In the 1980s, the abortion–breast cancer hypothesis posited that induced abortion increased the risk of developing breast cancer.[67] This hypothesis was the subject of extensive scientific inquiry, which concluded that neither miscarriages nor abortions are associated with a heightened risk for breast cancer.[68]
Other risk factors include radiation[69] and circadian disruptions related to shift-work[70] and routine late-night eating.[71] A number of chemicals have also been linked, including polychlorinated biphenyls, polycyclic aromatic hydrocarbons, and organic solvents[72] Although the radiation from mammography is a low dose, it is estimated that yearly screening from 40 to 80 years of age will cause approximately 225 cases of fatal breast cancer per million women screened.[73]
Hormone therapy and hormonal contraception
In general, hormone replacement therapy (HRT) to treat menopause is associated with only a small increased risk of breast cancer.[74][75][76] The level of risk also depends on the type of HRT, the duration of the treatment and the age of the person. Oestrogen-only HRT, taken by people who had a hysterectomy, comes with an extremely low level of breast cancer risk. The most commonly taken combined HRT (oestrogen and progestogen) is linked to a small risk of breast cancer. This risk is lower for women in their 50s and higher for older women. The risk increases with the duration of HRT. When HRT is taken for a year or less, there is no increased risk of breast cancer. HRT taken for more than 5 years comes with an increased risk but the risk reduces after the therapy is stopped.[75][76]
The use of hormonal birth control does not cause breast cancer for most women;[77] if it has an effect, it is small (on the order of 0.01% per user–year; comparable to the rate of maternal mortality in the United States[78]), temporary, and offset by the users' significantly reduced risk of ovarian and endometrial cancers.[78] Among those with a family history of breast cancer, use of modern oral contraceptives does not appear to affect the risk of breast cancer.[79] It is less certain whether hormonal contraceptives could increase the already high rates of breast cancer in women with mutations in the breast cancer susceptibility genes BRCA1 or BRCA2.[80]
Genetics
Genetics is believed to be the primary cause of 5–10% of all cases.[81] Women whose mother was diagnosed before 50 have an increased risk of 1.7 and those whose mother was diagnosed at age 50 or after has an increased risk of 1.4.[82] In those with zero, one or two affected relatives, the risk of breast cancer before the age of 80 is 7.8%, 13.3%, and 21.1% with a subsequent mortality from the disease of 2.3%, 4.2%, and 7.6% respectively.[83] In those with a first degree relative with the disease the risk of breast cancer between the age of 40 and 50 is double that of the general population.[84]
In less than 5% of cases, genetics plays a more significant role by causing a hereditary breast–ovarian cancer syndrome.[85] This includes those who carry the BRCA1 and BRCA2 gene mutation.[85] These mutations account for up to 90% of the total genetic influence with a risk of breast cancer of 60–80% in those affected.[81] Other significant mutations include p53 (Li–Fraumeni syndrome), PTEN (Cowden syndrome), and STK11 (Peutz–Jeghers syndrome), CHEK2, ATM, BRIP1, and PALB2.[81] In 2012, researchers said that there are four genetically distinct types of the breast cancer and that in each type, hallmark genetic changes lead to many cancers.[86]
Other genetic predispositions include the density of the breast tissue and hormonal levels. Women with dense breast tissue are more likely to get tumours and are less likely to be diagnosed with breast cancer – because the dense tissue makes tumours less visible on mammograms. Furthermore, women with naturally high estrogen and progesterone levels are also at higher risk for tumour development.[87][88]
Medical conditions
Breast changes like atypical ductal hyperplasia[89] and lobular carcinoma in situ,[90][91] found in benign breast conditions such as fibrocystic breast changes, are correlated with an increased breast cancer risk.
Diabetes mellitus might also increase the risk of breast cancer.[92] Autoimmune diseases such as lupus erythematosus seem also to increase the risk for the acquisition of breast cancer.[93]
The major causes of sporadic breast cancer are associated with hormone levels. Breast cancer is promoted by estrogen. This hormone activates the development of breast throughout puberty, menstrual cycles and pregnancy. The imbalance between estrogen and progesterone during the menstrual phases causes cell proliferation. Moreover, oxidative metabolites of estrogen can increase DNA damage and mutations. Repeated cycling and the impairment of repair process can transform a normal cell into pre-malignant and eventually malignant cell through mutation. During the premalignant stage, high proliferation of stromal cells can be activated by estrogen to support the development of breast cancer. During the ligand binding activation, the ER can regulate gene expression by interacting with estrogen response elements within the promotor of specific genes. The expression and activation of ER due to lack of estrogen can be stimulated by extracellular signals.[94] Interestingly, the ER directly binding with the several proteins, including growth factor receptors, can promote the expression of genes related to cell growth and survival.[95]
Raised prolactin levels in the blood are associated with increased risk of breast cancer.[96] A meta-analysis of observational research with over two million individuals has suggested a moderate association of antipsychotic use with breast cancer, possibly mediated by prolactin-inducing properties of specific agents.[97]
Pathophysiology

Breast cancer, like other cancers, occurs because of an interaction between an environmental (external) factor and a genetically susceptible host. Normal cells divide as many times as needed and stop. They attach to other cells and stay in place in tissues. Cells become cancerous when they lose their ability to stop dividing, to attach to other cells, to stay where they belong, and to die at the proper time.
Normal cells will self-destruct (programmed cell death) when they are no longer needed. Until then, cells are protected from programmed death by several protein clusters and pathways. One of the protective pathways is the PI3K/AKT pathway; another is the RAS/MEK/ERK pathway. Sometimes the genes along these protective pathways are mutated in a way that turns them permanently "on", rendering the cell incapable of self-destructing when it is no longer needed. This is one of the steps that causes cancer in combination with other mutations. Normally, the PTEN protein turns off the PI3K/AKT pathway when the cell is ready for programmed cell death. In some breast cancers, the gene for the PTEN protein is mutated, so the PI3K/AKT pathway is stuck in the "on" position, and the cancer cell does not self-destruct.[98]
Mutations that can lead to breast cancer have been experimentally linked to estrogen exposure.[99] Additionally, G-protein coupled estrogen receptors have been associated with various cancers of the female reproductive system including breast cancer.[100]
Abnormal growth factor signaling in the interaction between stromal cells and epithelial cells can facilitate malignant cell growth.[101][102] In breast adipose tissue, overexpression of leptin leads to increased cell proliferation and cancer.[103]
In the United States, 10 to 20 percent of women with breast cancer or ovarian cancer have a first- or second-degree relative with one of these diseases. Men with breast cancer have an even higher likelihood. The familial tendency to develop these cancers is called hereditary breast–ovarian cancer syndrome. The best known of these, the BRCA mutations, confer a lifetime risk of breast cancer of between 60 and 85 percent and a lifetime risk of ovarian cancer of between 15 and 40 percent. Some mutations associated with cancer, such as p53, BRCA1 and BRCA2, occur in mechanisms to correct errors in DNA. These mutations are either inherited or acquired after birth. Presumably, they allow further mutations, which allow uncontrolled division, lack of attachment, and metastasis to distant organs.[69][104] However, there is strong evidence of residual risk variation that goes well beyond hereditary BRCA gene mutations between carrier families. This is caused by unobserved risk factors.[105] This implicates environmental and other causes as triggers for breast cancers. The inherited mutation in BRCA1 or BRCA2 genes can interfere with repair of DNA cross links and DNA double strand breaks (known functions of the encoded protein).[106] These carcinogens cause DNA damage such as DNA cross links and double strand breaks that often require repairs by pathways containing BRCA1 and BRCA2.[107][108] However, mutations in BRCA genes account for only 2 to 3 percent of all breast cancers.[109] Levin et al. say that cancer may not be inevitable for all carriers of BRCA1 and BRCA2 mutations.[110] About half of hereditary breast–ovarian cancer syndromes involve unknown genes. Furthermore, certain latent viruses, may decrease the expression of the BRCA1 gene and increase the risk of breast tumours.[111]
GATA-3 directly controls the expression of estrogen receptor (ER) and other genes associated with epithelial differentiation, and the loss of GATA-3 leads to loss of differentiation and poor prognosis due to cancer cell invasion and metastasis.[112]
Screening
Breast cancer screening refers to testing otherwise-healthy women for breast cancer in an attempt to diagnose breast tumors early when treatments are more successful. The most common screening test for breast cancer is low-dose X-ray imaging of the breast, called mammography.[113] Each breast is pressed between two plates and imaged. Tumors can appear unusually dense within the breast, distort the shape of surrounding tissue, or cause small dense flecks called microcalcifications.[114] Radiologists generally report mammogram results on a standardized scale – the six-point Breast Imaging-Reporting and Data System (BI-RADS) is the most common globally – where a higher number corresponds to a greater risk of a cancerous tumor.[115][116]
A mammogram also reveals breast density; dense breast tissue appears opaque on a mammogram and can obscure tumors.[117][118] BI-RADS categorizes breast density into four categories. Mammography can detect around 90% of breast tumors in the least dense breasts (called "fatty" breasts), but just 60% in the most dense breasts (called "extremely dense").[119] Women with particularly dense breasts can instead be screened by ultrasound, magnetic resonance imaging (MRI), or tomosynthesis, all of which more sensitively detect breast tumors.[120]
Regular screening mammography reduces breast cancer deaths by at least 20%.[121] Most medical guidelines recommend annual screening mammograms for women aged 50–70.[122] Screening also reduces breast cancer mortality in women aged 40–49, and some guidelines recommend annual screening in this age group as well.[122][123] For women at high risk for developing breast cancer, most guidelines recommend adding MRI screening to mammography, to increase the chance of detecting potentially dangerous tumors.[120] Regularly feeling one's own breasts for lumps or other abnormalities, called breast self-examination, does not reduce a person's chance of dying from breast cancer.[124] Clinical breast exams, where a health professional feels the breasts for abnormalities, are common;[125] whether they reduce the risk of dying from breast cancer is not known.[113]
For the average woman, the U.S. Preventive Services Task Force and American College of Physicians recommends mammography every two years in women between the ages of 50 and 74,[12][126] the Council of Europe recommends mammography between 50 and 69 with most programs using a 2-year frequency,[127] while the European Commission recommends mammography from 45 to 75 every 2 to 3 years,[128] and in Canada screening is recommended between the ages of 50 and 74 at a frequency of 2 to 3 years.[129] The American Cancer Society also endorses that women ages 40 and older receive mammograms annually.[130] These task force reports point out that in addition to unnecessary surgery and anxiety, the risks of more frequent mammograms include a small but significant increase in breast cancer induced by radiation.[131]
Diagnosis

Those who have a suspected tumor from a mammogram or physical exam first undergo additional imaging – typically a second "diagnostic" mammogram and ultrasound – to confirm its presence and location.[19] A biopsy is then taken of the suspected tumor. Breast biopsy is typically done by core needle biopsy, with a hollow needle used to collect tissue from the area of interest.[132] Suspected tumors that appear to be filled with fluid are often instead sampled by fine-needle aspiration.[132][133] Around 10–20% of breast biopsies are positive for cancer.[134]
 MRI showing breast cancer
MRI showing breast cancer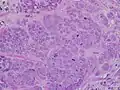 High-grade invasive ductal carcinoma, with minimal tubule formation, marked pleomorphism, and prominent mitoses, 40x field
High-grade invasive ductal carcinoma, with minimal tubule formation, marked pleomorphism, and prominent mitoses, 40x field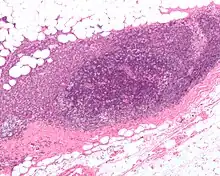 Micrograph showing a lymph node invaded by ductal breast carcinoma, with an extension of the tumor beyond the lymph node
Micrograph showing a lymph node invaded by ductal breast carcinoma, with an extension of the tumor beyond the lymph node_expression_in_normal_breast_and_breast_carcinoma_tissue.jpg.webp) Neuropilin-2 expression in normal breast and breast carcinoma tissue
Neuropilin-2 expression in normal breast and breast carcinoma tissue F-18 FDG PET/CT: A breast cancer metastasis to the right scapula
F-18 FDG PET/CT: A breast cancer metastasis to the right scapula Elastography shows stiff cancer tissue on ultrasound imaging.
Elastography shows stiff cancer tissue on ultrasound imaging.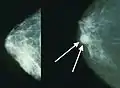 Mammograms showing a normal breast (left) and a breast with cancer (right)
Mammograms showing a normal breast (left) and a breast with cancer (right)
Classification
Breast cancers are classified by several grading systems. Each of these influences the prognosis and can affect treatment response. Description of a breast cancer optimally includes all of these factors.

- Histopathology. Breast cancer is usually classified primarily by its histological appearance. Most breast cancers are derived from the epithelium lining the ducts or lobules, and these cancers are classified as ductal or lobular carcinoma. Carcinoma in situ is growth of low-grade cancerous or precancerous cells within a particular tissue compartment such as the mammary duct without invasion of the surrounding tissue. In contrast, invasive carcinoma does not confine itself to the initial tissue compartment.[135]
- Grade. Grading compares the appearance of the breast cancer cells to the appearance of normal breast tissue. Normal cells in an organ like the breast become differentiated, meaning that they take on specific shapes and forms that reflect their function as part of that organ. Cancerous cells lose that differentiation. In cancer, the cells that would normally line up in an orderly way to make up the milk ducts become disorganized. Cell division becomes uncontrolled. Cell nuclei become less uniform. Pathologists describe cells as well differentiated (low grade), moderately differentiated (intermediate grade), and poorly differentiated (high grade) as the cells progressively lose the features seen in normal breast cells. Poorly differentiated cancers (the ones whose tissue is least like normal breast tissue) have a worse prognosis.
- Stage. Breast cancer staging using the TNM system is based on the size of the tumour (T), whether or not the tumour has spread to the lymph nodes (N) in the armpits, and whether the tumour has metastasized (M) (i.e. spread to a more distant part of the body). Larger size, nodal spread, and metastasis have a larger stage number and a worse prognosis.
The main stages are:- Stage 0 is a pre-cancerous or marker condition, either ductal carcinoma in situ (DCIS) or lobular carcinoma in situ (LCIS).
- Stages 1–3 are within the breast or regional lymph nodes.
- Stage 4 is 'metastatic' cancer that has a less favorable prognosis since it has spread beyond the breast and regional lymph nodes.
 Stage T1 breast cancer
Stage T1 breast cancer Stage T2 breast cancer
Stage T2 breast cancer Stage T3 breast cancer
Stage T3 breast cancer Metastatic or stage 4 breast cancer
Metastatic or stage 4 breast cancer
- Where available, imaging studies may be employed as part of the staging process in select cases to look for signs of metastatic cancer. However, in cases of breast cancer with low risk for metastasis, the risks associated with PET scans, CT scans, or bone scans outweigh the possible benefits, as these procedures expose the person to a substantial amount of potentially dangerous ionizing radiation.[136][137]
- Receptor status. Breast cancer cells have receptors on their surface and in their cytoplasm and nucleus. Chemical messengers such as hormones bind to receptors, and this causes changes in the cell. Breast cancer cells may or may not have three important receptors: estrogen receptor (ER), progesterone receptor (PR), and HER2.
ER+ cancer cells (that is, cancer cells that have estrogen receptors) depend on estrogen for their growth, so they can be treated with drugs to block estrogen effects (e.g. tamoxifen), and generally have a better prognosis. Untreated, HER2+ breast cancers are generally more aggressive than HER2- breast cancers,[138][139] but HER2+ cancer cells respond to drugs such as the monoclonal antibody trastuzumab (in combination with conventional chemotherapy), and this has improved the prognosis significantly.[140] Cells that do not have any of these three receptor types (estrogen receptors, progesterone receptors, or HER2) are called triple-negative, although they frequently do express receptors for other hormones, such as androgen receptor and prolactin receptor. - DNA assays. DNA testing of various types including DNA microarrays have compared normal cells to breast cancer cells. The specific changes in a particular breast cancer can be used to classify the cancer in several ways, and may assist in choosing the most effective treatment for that DNA type.
 Stage 1A breast cancer
Stage 1A breast cancer Stage 1B breast cancer
Stage 1B breast cancer Stage 2A breast cancer
Stage 2A breast cancer Stage 2A breast cancer
Stage 2A breast cancer Stage 2B breast cancer
Stage 2B breast cancer Stage 2B breast cancer
Stage 2B breast cancer Stage 2B breast cancer
Stage 2B breast cancer Stage 3A breast cancer
Stage 3A breast cancer Stage 3A breast cancer
Stage 3A breast cancer Stage 3A breast cancer
Stage 3A breast cancer Stage 3B breast cancer
Stage 3B breast cancer Stage 3B breast cancer
Stage 3B breast cancer Stage 4 breast cancer
Stage 4 breast cancer
Prevention
Lifestyle
Women can reduce their risk of breast cancer by maintaining a healthy weight, reducing alcohol use, increasing physical activity, and breast-feeding.[141] These modifications might prevent 38% of breast cancers in the US, 42% in the UK, 28% in Brazil, and 20% in China.[141] The benefits with moderate exercise such as brisk walking are seen at all age groups including postmenopausal women.[141][142] High levels of physical activity reduce the risk of breast cancer by about 14%.[143] Strategies that encourage regular physical activity and reduce obesity could also have other benefits, such as reduced risks of cardiovascular disease and diabetes.[41] A study that included data from 130,957 women of European ancestry found "strong evidence that greater levels of physical activity and less sedentary time are likely to reduce breast cancer risk, with results generally consistent across breast cancer subtypes".[144]
The American Cancer Society and the American Society of Clinical Oncology advised in 2016 that people should eat a diet high in vegetables, fruits, whole grains, and legumes.[145] Eating foods rich in soluble fiber contributes to reducing breast cancer risk.[146][147] High intake of citrus fruit has been associated with a 10% reduction in the risk of breast cancer.[148] Marine omega-3 polyunsaturated fatty acids appear to reduce the risk.[149] High consumption of soy-based foods may reduce risk.[150]
Pre-emptive surgery
Removal of both breasts before any cancer has been diagnosed or any suspicious lump or other lesion has appeared (a procedure known as "prophylactic bilateral mastectomy" or "risk reducing mastectomy") may be considered in women with BRCA1 and BRCA2 mutations, which are associated with a substantially heightened risk for an eventual diagnosis of breast cancer.[151][152] Evidence is not strong enough to support this procedure in anyone but women at the highest risk.[153] BRCA testing is recommended in those with a high family risk after genetic counseling. It is not recommended routinely.[154] This is because there are many forms of changes in BRCA genes, ranging from harmless polymorphisms to obviously dangerous frameshift mutations.[154] The effect of most of the identifiable changes in the genes is uncertain. Testing in an average-risk person is particularly likely to return one of these indeterminate, useless results. Removing the second breast in a person who has breast cancer (contralateral risk‐reducing mastectomy or CRRM) may reduce the risk of cancer in the second breast, however, it is unclear if removing the second breast in those who have breast cancer improves survival.[153] An increasing number women who test positive for faulty BRCA1 or BRCA2 genes choose to have risk-reducing surgery. At the same time the average waiting time for undergoing the procedure is two-years which is much longer than recommended.[155][156]
Medications
The selective estrogen receptor modulators reduce the risk of breast cancer but increase the risk of thromboembolism and endometrial cancer.[157] There is no overall change in the risk of death.[157][158] They are thus not recommended for the prevention of breast cancer in women at average risk but it is recommended they be offered for those at high risk and over the age of 35.[159] The benefit of breast cancer reduction continues for at least five years after stopping a course of treatment with these medications.[160] Aromatase inhibitors (such as exemestane and anastrozole) may be more effective than selective estrogen receptor modulators (such as tamoxifen) at reducing breast cancer risk and they are not associated with an increased risk of endometrial cancer and thromboembolism.[161]
Management
The management of breast cancer depends on various factors, including the stage of the cancer and the person's age. Treatments are more aggressive when the cancer is more advanced or there is a higher risk of recurrence of the cancer following treatment.
Breast cancer is usually treated with surgery, which may be followed by chemotherapy or radiation therapy, or both. A multidisciplinary approach is preferable.[162] Hormone receptor-positive cancers are often treated with hormone-blocking therapy over courses of several years. Monoclonal antibodies, or other immune-modulating treatments, may be administered in certain cases of metastatic and other advanced stages of breast cancer, although this range of treatment is still being studied.[163]
Surgery

Surgery involves the physical removal of the tumour, typically along with some of the surrounding tissue. One or more lymph nodes may be biopsied during the surgery; increasingly the lymph node sampling is performed by a sentinel lymph node biopsy.
Standard surgeries include:
- Mastectomy: Removal of the whole breast.
- Quadrantectomy: Removal of one-quarter of the breast.
- Lumpectomy: Removal of a small part of the breast.
Once the tumour has been removed, if the person desires, breast reconstruction surgery, a type of plastic surgery, may then be performed to improve the aesthetic appearance of the treated site. Alternatively, women use breast prostheses to simulate a breast under clothing, or choose a flat chest. Nipple prosthesis can be used at any time following the mastectomy.
Medication
Medications used after and in addition to surgery are called adjuvant therapy. Chemotherapy or other types of therapy prior to surgery are called neoadjuvant therapy. Aspirin may reduce mortality from breast cancer when used with other treatments.[164][165]
There are currently three main groups of medications used for adjuvant breast cancer treatment: hormone-blocking agents, chemotherapy, and monoclonal antibodies.
Hormonal therapy
Some breast cancers require estrogen to continue growing. They can be identified by the presence of estrogen receptors (ER+) and progesterone receptors (PR+) on their surface (sometimes referred to together as hormone receptors). These ER+ cancers can be treated with drugs that either block the receptors, e.g. tamoxifen, or alternatively block the production of estrogen with an aromatase inhibitor, e.g. anastrozole[166] or letrozole. The use of tamoxifen is recommended for 10 years.[167] Tamoxifen increases the risk of postmenopausal bleeding, endometrial polyps, hyperplasia, and endometrial cancer; using tamoxifen with an intrauterine system releasing levonorgestrel might increase vaginal bleeding after one to two years, but reduces somewhat endometrial polyps and hyperplasia, but not necessarily endometrial cancer.[168] Letrozole is recommended for five years.
Aromatase inhibitors are only suitable for women after menopause; however, in this group, they appear better than tamoxifen.[169] This is because the active aromatase in postmenopausal women is different from the prevalent form in premenopausal women, and therefore these agents are ineffective in inhibiting the predominant aromatase of premenopausal women.[170] Aromatase inhibitors should not be given to premenopausal women with intact ovarian function (unless they are also on treatment to stop their ovaries from working).[171] CDK inhibitors can be used in combination with endocrine or aromatase therapy.[172]
Chemotherapy
Chemotherapy is predominantly used for cases of breast cancer in stages 2–4, and is particularly beneficial in estrogen receptor-negative (ER-) disease. The chemotherapy medications are administered in combinations, usually for periods of 3–6 months. One of the most common regimens, known as "AC", combines cyclophosphamide with doxorubicin. Sometimes a taxane drug, such as docetaxel, is added, and the regime is then known as "CAT". Another common treatment is cyclophosphamide, methotrexate, and fluorouracil (or "CMF"). Most chemotherapy medications work by destroying fast-growing and/or fast-replicating cancer cells, either by causing DNA damage upon replication or by other mechanisms. However, the medications also damage fast-growing normal cells, which may cause serious side effects. Damage to the heart muscle is the most dangerous complication of doxorubicin, for example.
Monoclonal antibodies
Trastuzumab, a monoclonal antibody to HER2, has improved the five-year disease free survival of stage 1–3 HER2-positive breast cancers to about 87% (overall survival 95%).[173] Between 25% and 30% of breast cancers overexpress the HER2 gene or its protein product,[174] and overexpression of HER2 in breast cancer is associated with increased disease recurrence and worse prognosis. Trastuzumab, however, is very expensive, and its use may cause serious side effects (approximately 2% of people who receive it develop significant heart damage).[175] Another antibody pertuzumab prevents HER2 dimerization and is recommended together with trastuzumab and chemotherapy in severe disease.[176][177]
Targeted therapy
Elacestrant (Orserdu) was approved for medical use in the United States in January 2023.[178][179]
Capivasertib (Truqap) was approved for medical use in the United States in November 2023.[180][181][182]
Radiation

Radiotherapy is given after surgery to the region of the tumour bed and regional lymph nodes, to destroy microscopic tumour cells that may have escaped surgery. When given intraoperatively as targeted intraoperative radiotherapy, it may also have a beneficial effect on tumour microenvironment.[183][184] Radiation therapy can be delivered as external beam radiotherapy or as brachytherapy (internal radiotherapy). Conventionally radiotherapy is given after the operation for breast cancer. Radiation can also be given at the time of operation on the breast cancer. Radiation can reduce the risk of recurrence by 50–66% (1/2 – 2/3 reduction of risk) when delivered in the correct dose[185] and is considered essential when breast cancer is treated by removing only the lump (Lumpectomy or Wide local excision). In early breast cancer, partial breast irradiation does not give the same cancer control in the breast as treating the whole breast and may cause worse side effects.[186]
Follow-up care
Care after primary breast cancer treatment, otherwise called 'follow-up care', can be intensive involving regular laboratory tests in asymptomatic people to try to achieve earlier detection of possible metastases. A review has found that follow-up programs involving regular physical examinations and yearly mammography alone are as effective as more intensive programs consisting of laboratory tests in terms of early detection of recurrence, overall survival and quality of life.[187]
Multidisciplinary rehabilitation programmes, often including exercise, education and psychological help, may produce short-term improvements in functional ability, psychosocial adjustment and social participation in people with breast cancer.[188]
Upper limb problems such as shoulder and arm pain, weakness and restricted movement are a common side effect after radiotherapy or breast cancer surgery.[189] According to research in the UK, an exercise programme started 7–10 days after surgery can reduce upper limb problems.[190][191]
Prognosis

Prognostic factors
| Stage | 5-year survival |
|---|---|
| Stage I | 100% |
| Stage II | 90% |
| Stage III | 70% |
| Stage IV | 30% |
The stage of the breast cancer is the most important component of traditional classification methods of breast cancer, because it has a greater effect on the prognosis than the other considerations. Staging takes into consideration size, local involvement, lymph node status and whether metastatic disease is present. The higher the stage at diagnosis, the poorer the prognosis. The stage is raised by the invasiveness of disease to lymph nodes, chest wall, skin or beyond, and the aggressiveness of the cancer cells. The stage is lowered by the presence of cancer-free zones and close-to-normal cell behaviour (grading). Size is not a factor in staging unless the cancer is invasive. For example, ductal carcinoma in situ (DCIS) involving the entire breast will still be stage zero and consequently an excellent prognosis.
- Stage 1 cancers (and DCIS, LCIS) have an excellent prognosis and are generally treated with lumpectomy and sometimes radiation.[193]
- Stage 2 and 3 cancers with a progressively poorer prognosis and greater risk of recurrence are generally treated with surgery (lumpectomy or mastectomy with or without lymph node removal), chemotherapy (plus trastuzumab for HER2+ cancers) and sometimes radiation (particularly following large cancers, multiple positive nodes or lumpectomy).
- Stage 4, metastatic cancer, (i.e. spread to distant sites) has a poor prognosis and is managed by various combination of all treatments from surgery, radiation, chemotherapy and targeted therapies.
The breast cancer grade is assessed by comparison of the breast cancer cells to normal breast cells. The closer to normal the cancer cells are, the slower their growth and the better the prognosis. If cells are not well differentiated, they will appear immature, will divide more rapidly, and will tend to spread. Well differentiated is given a grade of 1, moderate is grade 2, while poor or undifferentiated is given a higher grade of 3 or 4 (depending upon the scale used). The most widely used grading system is the Nottingham scheme.[194]
Younger women with an age of less than 40 years or women over 80 years tend to have a poorer prognosis than post-menopausal women due to several factors. Their breasts may change with their menstrual cycles, they may be nursing infants, and they may be unaware of changes in their breasts. Therefore, younger women are usually at a more advanced stage when diagnosed. There may also be biological factors contributing to a higher risk of disease recurrence for younger women with breast cancer.[195]
Psychological aspects
Not all people with breast cancer experience their illness in the same manner. Factors such as age can have a significant impact on the way a person copes with a breast cancer diagnosis. Premenopausal women with estrogen-receptor positive breast cancer must confront the issues of early menopause induced by many of the chemotherapy regimens used to treat their breast cancer, especially those that use hormones to counteract ovarian function.[196]
In women with non-metastatic breast cancer, psychological interventions such as cognitive behavioral therapy can have positive effects on outcomes such as anxiety, depression and mood disturbance, and can also improve the quality of life.[197] Physical activity interventions may also have beneficial effects on health related quality of life, anxiety, fitness and physical activity in women with breast cancer following adjuvant therapy.[198]
Cardiovascular outcomes in breast cancer survivors
With nearly 3 million BC survivors in the USA,[199] the 5-year survival rate for patients has increased to over 90% thanks to advancements in breast cancer treatment and earlier detection.[200] Cardiovascular diseases (CVD) are becoming more widely acknowledged as a significant cause of morbidity and mortality as breast cancer patients live longer.[201]
The recent meta-analysis compared the risk of developing cardiovascular disease in breast cancer patients to the risk in a general matched cancer-free population, and also estimated the incidence of cardiovascular events in BC patients.[202] After analysing data from 26 studies (836,301 patients), the authors found that breast cancer survivors demonstrated a higher risk for cardiovascular death within five years of cancer diagnosis (HR = 1.09; 95% CI: 1.07, 1.11), HF within ten years (HR = 1.21; 95% CI: 1.1, 1.33), and AF within three years (HR = 1.13; 95% CI: 1.05, 1.21).[202]
The epidemiological data from 2,111,882 breast cancer patients revealed that the pooled incidence rates for cardiovascular death was 1.73 (95% CI 1.18, 2.53), 4.44 (95% CI 3.33, 5.92) for heart failure, 4.29 (95% CI 3.09, 5.94) for coronary artery disease, 1.98 (95% CI 1.24, 3.16) for myocardial infarction, 4.33 (95% CI 2.97, 6.30) for stroke of any type, and 2.64 (95% CI 2.97, 6.30) for ischemic stroke per 1000 person-years of follow-up.[202] The study clearly highlighted the crucial need for clinicians to thoroughly examine the cardiovascular risk factor profile of breast cancer survivors and monitor their cardiovascular health.[202]
Epidemiology

|
no data
<2
2–4
4–6
6–8
8–10
10–12 |
12–14
14–16
16–18
18–20
20–22
>22
|
Breast cancer is the most-common invasive cancer in women,[204] accounting for 30% of cancer cases in women.[205] Along with lung cancer, breast cancer is the most commonly diagnosed cancer, with 2.09 million cases each in 2018.[206] Breast cancer affects 1 in 7 (14%) of women worldwide.[207] (The most common form of cancer is non-invasive non-melanoma skin cancer; non-invasive cancers are generally easily cured, cause very few deaths, and are routinely excluded from cancer statistics.) In 2008, breast cancer caused 458,503 deaths worldwide (13.7% of cancer deaths in women and 6.0% of all cancer deaths for men and women together).[208] Lung cancer, the second most-common cause of cancer-related deaths in women, caused 12.8% of cancer deaths in women (18.2% of all cancer deaths for men and women together).[208]
The incidence of breast cancer varies greatly around the world: it is lowest in less-developed countries and greatest in the more-developed countries. In the twelve world regions, the annual age-standardized incidence rates per 100,000 women are as follows: 18 in Eastern Asia, 22 in South Central Asia and sub-Saharan Africa, 26 in South-Eastern Asia, 26, 28 in North Africa and Western Asia, 42 in South and Central America, 42, 49 in Eastern Europe, 56 in Southern Europe, 73 in Northern Europe, 74 in Oceania, 78 in Western Europe, and 90 in North America.[209] Metastatic breast cancer affects between 19% (United States) and 50% (parts of Africa) of women with breast cancer.[210]
The number of cases worldwide has significantly increased since the 1970s, a phenomenon partly attributed to the modern lifestyles.[211][212] Breast cancer is strongly related to age with only 5% of all breast cancers occurring in women under 40 years old.[213] There were more than 41,000 newly diagnosed cases of breast cancer registered in England in 2011, around 80% of these cases were in women age 50 or older.[214] Based on U.S. statistics in 2015 there were 2.8 million women affected by breast cancer.[204] In the United States, the age-adjusted incidence of breast cancer per 100,000 women rose from around 102 cases per year in the 1970s to around 141 in the late-1990s, and has since fallen, holding steady around 125 since 2003. However, age-adjusted deaths from breast cancer per 100,000 women only rose slightly from 31.4 in 1975 to 33.2 in 1989 and have since declined steadily to 20.5 in 2014.[215]
Multiple primary tumours

Multiple primary tumours can arise in different sites (as opposed to a single tumour spreading). These tumours can occur in both breasts (bilateral tumours), in different quadrants of a single breast (multi-centric cancer), or separate tumours within a single breast quadrant (multi-focal cancer).[216][217]
Incidence of multi-centric and multi-focal breast cancers (MMBC) is increasing, partly due to improving mammography technology.[218] Incidence of MMBC is reported between 9 and 75% in high income countries, depending on criteria used.[218] For instance, China reported that only 2% of patients are defined as MMBC.[218] The reason for this difference is due to lack of uniformity in diagnosis.[218] Therefore, standardised method and criteria should be made in order to define the incidence of MMBC correctly.[218]
Mutations in tumour suppressor genes such as BRCA1 and BRCA2, the PI3K/AKT/mTOR pathway and PTEN can be related to formation of multiple primary breast cancers.[219] Diagnosis occurs via the same modalities as other breast cancers.
Mastectomy is the standard surgical treatment for multi centric breast cancer patients.[220] Double lumpectomies, also labelled as breast conservative therapy (BCT), is an alternative and preferred surgical treatment to mastectomy for early stage multi centric breast cancer patients.[221] The procedure of double lumpectomies involves the surgical ablation of the cancerous tumour foci and the surrounding breast tissues in different quadrant of the same breast.[221] The benefits of double lumpectomies are the avoidance of breast reconstruction surgery and minimal breast scarring. However, it is not preferred for patients with more than two tumours within the same breast due to difficulty in removing all cancer cells.[222] Patients with multiple primary breast tumours may receive treatments such as chemotherapy, radiotherapy and breast reconstruction surgery[222][223] for the same indications as other breast cancer patients.
History
Because of its visibility, breast cancer was the form of cancer most often described in ancient documents.[224]: 9–13 Because autopsies were rare, cancers of the internal organs were essentially invisible to ancient medicine. Breast cancer, however, could be felt through the skin, and in its advanced state often developed into fungating lesions: the tumour would become necrotic (die from the inside, causing the tumour to appear to break up) and ulcerate through the skin, weeping fetid, dark fluid.[224]: 9–13
The oldest discovered evidence of breast cancer is from Egypt and dates back 4200 years, to the Sixth Dynasty.[225] The study of a woman's remains from the necropolis of Qubbet el-Hawa showed the typical destructive damage due to metastatic spread.[225] The Edwin Smith Papyrus describes eight cases of tumours or ulcers of the breast that were treated by cauterization. The writing says about the disease, "There is no treatment."[226] For centuries, physicians described similar cases in their practices, with the same conclusion. Ancient medicine, from the time of the Greeks through the 17th century, was based on humoralism, and thus believed that breast cancer was generally caused by imbalances in the fundamental fluids that controlled the body, especially an excess of black bile.[224]: 32 Alternatively it was seen as divine punishment.[227]
Mastectomy for breast cancer was performed at least as early as AD 548, when it was proposed by the court physician Aetios of Amida to Theodora.[224]: 9–13 It was not until doctors achieved greater understanding of the circulatory system in the 17th century that they could link breast cancer's spread to the lymph nodes in the armpit. In the early 18th century the French surgeon Jean Louis Petit performed total mastectomies that included removing the axillary lymph nodes, as he recognized that this reduced recurrence.[228] Petit's work built on the methods of the surgeon Bernard Peyrilhe, who in the 17th century additionally removed the pectoral muscle underlying the breast, as he judged that this greatly improved the prognosis.[229] But poor results and the considerable risk to the patient meant that physicians did not share the opinion of surgeons such as Nicolaes Tulp, who in the 17th century proclaimed "the sole remedy is a timely operation". The eminent surgeon Richard Wiseman documented in the mid 17th century that following 12 mastectomies, two patients died during the operation, eight patients died shortly after the operation from progressive cancer and only two of the 12 patients were cured.[230]: 6 Physicians were conservative in the treatment they prescribed in the early stages of breast cancer. Patients were treated with a mixture of detox purges, blood letting and traditional remedies that were supposed to lower acidity, such as the alkaline arsenic.[231]: 24
When in 1664 Anne of Austria was diagnosed with breast cancer, the initial treatment involved compresses saturated with hemlock juice. When the lumps increased the King's physician commenced a treatment with arsenic ointments.[231]: 25 The royal patient died 1666 in atrocious pain.[231]: 26 Each failing treatment for breast cancer led to the search for new treatments, spurring a market in remedies that were advertised and sold by quacks, herbalists, chemists and apothecaries.[232] The lack of anesthesia and antiseptics made mastectomy a painful and dangerous ordeal.[230] In the 18th century, a wide variety of anatomical discoveries were accompanied by new theories about the cause and growth of breast cancer. The investigative surgeon John Hunter claimed that neural fluid generated breast cancer. Other surgeons proposed that milk within the mammary ducts led to cancerous growths. Theories about trauma to the breast as cause for malignant changes in breast tissue were advanced. The discovery of breast lumps and swellings fueled controversies about hard tumours and whether lumps were benign stages of cancer. Medical opinion about necessary immediate treatment varied.[230]: 5 The surgeon Benjamin Bell advocated removal of the entire breast, even when only a portion was affected.[233]

Breast cancer was uncommon until the 19th century, when improvements in sanitation and control of deadly infectious diseases resulted in dramatic increases in lifespan. Previously, most women had died too young to have developed breast cancer.[234] In 1878, an article in Scientific American described historical treatment by pressure intended to induce local ischemia in cases when surgical removal were not possible.[235] William Stewart Halsted started performing radical mastectomies in 1882, helped greatly by advances in general surgical technology, such as aseptic technique and anesthesia. The Halsted radical mastectomy often involved removing both breasts, associated lymph nodes, and the underlying chest muscles. This often led to long-term pain and disability, but was seen as necessary to prevent the cancer from recurring.[224]: 102–106 Before the advent of the Halsted radical mastectomy, 20-year survival rates were only 10%; Halsted's surgery raised that rate to 50%.[224]: 1
Breast cancer staging systems were developed in the 1920s and 1930s to determining the extent to which a cancer has developed by growing and spreading.[224]: 102–106 The first case-controlled study on breast cancer epidemiology was done by Janet Lane-Claypon, who published a comparative study in 1926 of 500 breast cancer cases and 500 controls of the same background and lifestyle for the British Ministry of Health.[236] Radical mastectomies remained the standard of care in the USA until the 1970s, but in Europe, breast-sparing procedures, often followed by radiation therapy, were generally adopted in the 1950s.[224]: 102–106 In 1955 George Crile Jr. published Cancer and Common Sense arguing that cancer patients needed to understand available treatment options. Crile became a close friend of the environmentalist Rachel Carson, who had undergone a Halsted radical mastectomy in 1960 to treat her malign breast cancer.[237]: 39–40 The US oncologist Jerome Urban promoted superradical mastectomies, taking even more tissue, until 1963, when the ten-year survival rates proved equal to the less-damaging radical mastectomy.[224]: 102–106 Carson died in 1964 and Crile went on to published a wide variety of articles, both in the popular press and in medical journals, challenging the widespread used of the Halsted radical mastectomy. In 1973 Crile published What Women Should Know About the Breast Cancer Controversy. When in 1974 Betty Ford was diagnosed with breast cancer, the options for treating breast cancer were openly discussed in the press.[237]: 58 During the 1970s, a new understanding of metastasis led to perceiving cancer as a systemic illness as well as a localized one, and more sparing procedures were developed that proved equally effective.[238]
In the 1980s and 1990s, thousands of women who had successfully completed standard treatment then demanded and received high-dose bone marrow transplants, thinking this would lead to better long-term survival. However, it proved completely ineffective, and 15–20% of women died because of the brutal treatment.[239]: 200–203 The 1995 reports from the Nurses' Health Study and the 2002 conclusions of the Women's Health Initiative trial conclusively proved that hormone replacement therapy significantly increased the incidence of breast cancer.[239]
Society and culture
Before the 20th century, breast cancer was feared and discussed in hushed tones, as if it were shameful. As little could be safely done with primitive surgical techniques, women tended to suffer silently rather than seeking care. When surgery advanced, and long-term survival rates improved, women began raising awareness of the disease and the possibility of successful treatment. The "Women's Field Army", run by the American Society for the Control of Cancer (later the American Cancer Society) during the 1930s and 1940s was one of the first organized campaigns. In 1952, the first peer-to-peer support group, called "Reach to Recovery", began providing post-mastectomy, in-hospital visits from women who had survived breast cancer.[239]: 37–38
The breast cancer movement of the 1980s and 1990s developed out of the larger feminist movements and women's health movement of the 20th century.[239]: 4 This series of political and educational campaigns, partly inspired by the politically and socially effective AIDS awareness campaigns, resulted in the widespread acceptance of second opinions before surgery, less invasive surgical procedures, support groups, and other advances in care.[240]
Pink ribbon

A pink ribbon is the most prominent symbol of breast cancer awareness. Pink ribbons, which can be made inexpensively, are sometimes sold as fundraisers, much like poppies on Remembrance Day. They may be worn to honor those who have been diagnosed with breast cancer, or to identify products that the manufacturer would like to sell to consumers that are interested in breast cancer.[239]: 27–72 In the 1990s breast cancer awareness campaigns were launched by US based corporations. As part of these cause related marketing campaigns corporations donated to a variety of breast cancer initiatives for every pink ribbon product that was purchased.[241]>: 132–133 The Wall Street Journal noted "that the strong emotions provoked by breast cancer translate to a company's bottom line". While many US corporations donated to existing breast cancer initiatives others such as Avon established their own breast cancer foundations on the back of pink ribbon products.[241]: 135–136
Wearing or displaying a pink ribbon has been criticized by the opponents of this practice as a kind of slacktivism, because it has no practical positive effect. It has also been criticized as hypocrisy, because some people wear the pink ribbon to show good will towards women with breast cancer, but then oppose these women's practical goals, like patient rights and anti-pollution legislation.[239]: 366–368 [242] Critics say that the feel-good nature of pink ribbons and pink consumption distracts society from the lack of progress on preventing and curing breast cancer.[239]: 365–366 It is also criticized for reinforcing gender stereotypes and objectifying women and their breasts.<[239]: 372–374 In 2002 Breast Cancer Action launched the "Think Before You Pink" campaign against pinkwashing to target businesses that have co-opted the pink campaign to promote products that cause breast cancer, such as alcoholic beverages.[243]
Breast cancer culture
In her 2006 book Pink Ribbons, Inc.: Breast Cancer and the Politics of Philanthropy Samantha King claimed that breast cancer has been transformed from a serious disease and individual tragedy to a market-driven industry of survivorship and corporate sales pitch.[244] In 2010 Gayle Sulik argued that the primary purposes or goals of breast cancer culture are to maintain breast cancer's dominance as the pre-eminent women's health issue, to promote the appearance that society is doing something effective about breast cancer, and to sustain and expand the social, political, and financial power of breast cancer activists.[239]: 57 In the same year Barbara Ehrenreich published an opinion piece in Harper's Magazine, lamenting that in breast cancer culture, breast cancer therapy is viewed as a rite of passage rather than a disease. To fit into this mold, the woman with breast cancer needs to normalize and feminize her appearance, and minimize the disruption that her health issues cause anyone else. Anger, sadness, and negativity must be silenced. As with most cultural models, people who conform to the model are given social status, in this case as cancer survivors. Women who reject the model are shunned, punished and shamed. The culture is criticized for treating adult women like little girls, as evidenced by "baby" toys such as pink teddy bears given to adult women.[245]
Emphasis
In 2009 the US science journalist Christie Aschwanden criticized that the emphasis on breast cancer screening may be harming women by subjecting them to unnecessary radiation, biopsies, and surgery. One-third of diagnosed breast cancers might recede on their own.[246] Screening mammography efficiently finds non-life-threatening, asymptomatic breast cancers and precancers, even while overlooking serious cancers. According to the cancer researcher H. Gilbert Welch, screening mammography has taken the "brain-dead approach that says the best test is the one that finds the most cancers" rather than the one that finds dangerous cancers.[246]
In 2002 it was noted that as a result of breast cancer's high visibility, the statistical results can be misinterpreted, such as the claim that one in eight women will be diagnosed with breast cancer during their lives – a claim that depends on the unrealistic assumption that no woman will die of any other disease before the age of 95.[224]: 199–200 By 2010 the breast cancer survival rate in Europe was 91% at one years and 65% at five years. In the USA the five-year survival rate for localized breast cancer was 96.8%, while in cases of metastases it was only 20.6%. Because the prognosis for breast cancer was at this stage relatively favorable, compared to the prognosis for other cancers, breast cancer as cause of death among women was 13.9% of all cancer deaths. The second most common cause of death from cancer in women was lung cancer, the most common cancer worldwide for men and women. The improved survival rate made breast cancer the most prevalent cancer in the world. In 2010 an estimated 3.6 million women worldwide have had a breast cancer diagnosis in the past five years, while only 1.4 million male or female survivors from lung cancer were alive.[247]
Health disparities in breast cancer
There are ethnic disparities in the mortality rates for breast cancer as well as in breast cancer treatment. Breast cancer is the most prevalent cancer affecting women of every ethnic group in the United States. Breast cancer incidence among black women aged 45 and older is higher than that of white women in the same age group. White women aged 60–84 have higher incidence rates of breast cancer than Black women. Despite this, Black women at every age are more likely to succumb to breast cancer.[248]
Breast cancer treatment has improved greatly in recent years, but black women are still less likely to obtain treatment compared to white women.[248] Risk factors such as socioeconomic status, late-stage, or breast cancer at diagnosis, genetic differences in tumour subtypes, differences in health care access all contribute to these disparities. Socioeconomic determinants affecting the disparity in breast cancer illness include poverty, culture, as well as social injustice. In Hispanic women, the incidence of breast cancer is lower than in non-Hispanic women but is often diagnosed at a later stage than white women with larger tumors.
Black women are usually diagnosed with breast cancer at a younger age than white women. The median age of diagnosis for Black women is 59, in comparison to 62 in White women. The incidence of breast cancer in Black women has increased by 0.4% per year since 1975 and 1.5% per year among Asian/Pacific Islander women since 1992. Incidence rates were stable for non-Hispanic White, Hispanics, and Native women. The five-year survival rate is noted to be 81% in Black women and 92% in White women. Chinese and Japanese women have the highest survival rates.[248]
Poverty is a major driver for disparities related to breast cancer. Low-income women are less likely to undergo breast cancer screening and thus are more likely to have a late-stage diagnosis.[248] Ensuring women of all ethnic groups receive equitable health care including breast screening, can positively affect these disparities.[249]
Pregnancy
Pregnancy at an early age decreases the risk of developing breast cancer later in life.[250] The risk of breast cancer also declines with the number of children a woman has.[250] Breast cancer then becomes more common in the 5 or 10 years following pregnancy but then becomes less common than among the general population.[251] These cancers are known as postpartum breast cancer and have worse outcomes including an increased risk of distant spread of disease and mortality.[252] Other cancers found during or shortly after pregnancy appear at approximately the same rate as other cancers in women of a similar age.[253]
Diagnosing new cancer in a pregnant woman is difficult, in part because any symptoms are commonly assumed to be a normal discomfort associated with pregnancy.[253] As a result, cancer is typically discovered at a somewhat later stage than average in many pregnant or recently pregnant women. Some imaging procedures, such as MRIs (magnetic resonance imaging), CT scans, ultrasounds, and mammograms with fetal shielding are considered safe during pregnancy; some others, such as PET scans are not.[253]
Treatment is generally the same as for non-pregnant women.[253] However, radiation is normally avoided during pregnancy, especially if the fetal dose might exceed 100 cGy. In some cases, some or all treatments are postponed until after birth if the cancer is diagnosed late in the pregnancy. Early deliveries to speed the start of treatment are not uncommon. Surgery is generally considered safe during pregnancy, but some other treatments, especially certain chemotherapy drugs given during the first trimester, increase the risk of birth defects and pregnancy loss (spontaneous abortions and stillbirths).[253] Elective abortions are not required and do not improve the likelihood of the mother surviving or being cured.[253]
Radiation treatments may interfere with the mother's ability to breastfeed her baby because it reduces the ability of that breast to produce milk and increases the risk of mastitis. Also, when chemotherapy is being given after birth, many of the drugs pass through breast milk to the baby, which could harm the baby.[253]
Regarding future pregnancy among breast cancer survivors, there is often fear of cancer recurrence.[254] On the other hand, many still regard pregnancy and parenthood to represent normality, happiness and life fulfillment.[254]
Hormones
Birth control
In breast cancer survivors, non-hormonal birth control methods such as the copper intrauterine device (IUD) should be used as first-line options.[255] Progestogen-based methods such as depot medroxyprogesterone acetate, IUD with progestogen or progestogen only pills have a poorly investigated but possible increased risk of cancer recurrence, but may be used if positive effects outweigh this possible risk.[256]
Menopausal hormone replacement
In breast cancer survivors, it is recommended to first consider non-hormonal options for menopausal effects, such as bisphosphonates or selective estrogen receptor modulators (SERMs) for osteoporosis, and vaginal estrogen for local symptoms. Observational studies of systemic hormone replacement therapy after breast cancer are generally reassuring. If hormone replacement is necessary after breast cancer, estrogen-only therapy or estrogen therapy with an intrauterine device with progestogen may be safer options than combined systemic therapy.[257]
Research
Treatments are being evaluated in clinical trials. This includes individual drugs, combinations of drugs, and surgical and radiation techniques Investigations include new types of targeted therapy,[258] cancer vaccines, oncolytic virotherapy,[259] gene therapy[260][261] and immunotherapy.[262]
The latest research is reported annually at scientific meetings such as that of the American Society of Clinical Oncology, San Antonio Breast Cancer Symposium,[263] and the St. Gallen Oncology Conference in St. Gallen, Switzerland.[264] These studies are reviewed by professional societies and other organizations, and formulated into guidelines for specific treatment groups and risk category.
Fenretinide, a retinoid, is also being studied as a way to reduce the risk of breast cancer.[265][266] In particular, combinations of ribociclib plus endocrine therapy have been the subject of clinical trials.[267]
A 2019 review found moderate certainty evidence that giving people antibiotics before breast cancer surgery helped to prevent surgical site infection (SSI). Further study is required to determine the most effective antibiotic protocol and use in women undergoing immediate breast reconstruction.[268]
Cryoablation
As of 2014 cryoablation is being studied to see if it could be a substitute for a lumpectomy in small cancers.[269] There is tentative evidence in those with tumours less than 2 centimeters.[270] It may also be used in those in who surgery is not possible.[270] Another review states that cryoablation looks promising for early breast cancer of small size.[271]
Breast cancer cell lines
Part of the current knowledge on breast carcinomas is based on in vivo and in vitro studies performed with cell lines derived from breast cancers. These provide an unlimited source of homogenous self-replicating material, free of contaminating stromal cells, and often easily cultured in simple standard media. The first breast cancer cell line described, BT-20, was established in 1958. Since then, and despite sustained work in this area, the number of permanent lines obtained has been strikingly low (about 100). Indeed, attempts to culture breast cancer cell lines from primary tumours have been largely unsuccessful. This poor efficiency was often due to technical difficulties associated with the extraction of viable tumour cells from their surrounding stroma. Most of the available breast cancer cell lines issued from metastatic tumours, mainly from pleural effusions. Effusions provided generally large numbers of dissociated, viable tumour cells with little or no contamination by fibroblasts and other tumour stroma cells. Many of the currently used BCC lines were established in the late 1970s. A very few of them, namely MCF-7, T-47D, MDA-MB-231 and SK-BR-3, account for more than two-thirds of all abstracts reporting studies on mentioned breast cancer cell lines, as concluded from a Medline-based survey.
Molecular markers
Metabolic markers
Clinically, the most useful metabolic markers in breast cancer are the estrogen and progesterone receptors that are used to predict response to hormone therapy. New or potentially new markers for breast cancer include BRCA1 and BRCA2[272] to identify people at high risk of developing breast cancer, HER-2, and SCD1, for predicting response to therapeutic regimens, and urokinase plasminogen activator, PA1-1 and SCD1 for assessing prognosis.
Other animals
- Mammary tumor for breast cancer in other animals
- Mouse models of breast cancer metastasis
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Breast Cancer Treatment (PDQ®)". NCI. 23 May 2014. Archived from the original on 5 July 2014. Retrieved 29 June 2014.
- 1 2 3 4 5 6 7 8 World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 5.2. ISBN 978-92-832-0429-9.
- ↑ "Klinefelter Syndrome". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 24 May 2007. Archived from the original on 27 November 2012.
- 1 2 "SEER Stat Fact Sheets: Breast Cancer". NCI. Archived from the original on 3 July 2014. Retrieved 18 June 2014.
- 1 2 "Cancer Survival in England: Patients Diagnosed 2007–2011 and Followed up to 2012" (PDF). Office for National Statistics. 29 October 2013. Archived (PDF) from the original on 29 November 2014. Retrieved 29 June 2014.
- 1 2 Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (May 2021). "Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries". CA: A Cancer Journal for Clinicians. 71 (3): 209–249. doi:10.3322/caac.21660. PMID 33538338. S2CID 231804598.
- ↑ "Breast Cancer". NCI. January 1980. Archived from the original on 25 June 2014. Retrieved 29 June 2014.
- ↑ Saunders C, Jassal S (2009). Breast cancer (1. ed.). Oxford: Oxford University Press. p. Chapter 13. ISBN 978-0-19-955869-8. Archived from the original on 25 October 2015.
- ↑ Fakhri N, Chad MA, Lahkim M, Houari A, Dehbi H, Belmouden A, El Kadmiri N (September 2022). "Risk factors for breast cancer in women: an update review". Medical Oncology. 39 (12): 197. doi:10.1007/s12032-022-01804-x. PMID 36071255. S2CID 252113509.
- ↑ Gøtzsche PC, Jørgensen KJ (June 2013). "Screening for breast cancer with mammography". The Cochrane Database of Systematic Reviews. 2013 (6): CD001877. doi:10.1002/14651858.CD001877.pub5. PMC 6464778. PMID 23737396.
- ↑ Nelson HD, Tyne K, Naik A, Bougatsos C, Chan B, Nygren P, Humphrey L (November 2009). "Screening for Breast Cancer: Systematic Evidence Review Update for the US Preventive Services Task Force [Internet]". U.S. Preventive Services Task Force Evidence Syntheses. Rockville, MD: Agency for Healthcare Research and Quality. PMID 20722173. Report No.: 10-05142-EF-1.
- 1 2 Siu AL (February 2016). "Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement". Annals of Internal Medicine. 164 (4): 279–96. doi:10.7326/M15-2886. PMID 26757170.
- ↑ "Five Things Physicians and Patients Should Question". Choosing Wisely: an initiative of the ABIM Foundation. American College of Surgeons. September 2013. Archived from the original on 27 October 2013. Retrieved 2 January 2013.
- 1 2 3 4 "Breast Cancer Treatment (PDQ®)". NCI. 26 June 2014. Archived from the original on 5 July 2014. Retrieved 29 June 2014.
- 1 2 "World Cancer Report" (PDF). International Agency for Research on Cancer. 2008. Archived from the original (PDF) on 20 July 2011. Retrieved 26 February 2011.
- ↑ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 978-92-832-0429-9.
- ↑ Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (November 2018). "Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries". CA: A Cancer Journal for Clinicians. 68 (6): 394–424. doi:10.3322/caac.21492. PMID 30207593. S2CID 52188256.
- ↑ "Male Breast Cancer Treatment". National Cancer Institute. 2014. Archived from the original on 4 July 2014. Retrieved 29 June 2014.
- 1 2 Hayes & Lippman 2022, "Evaluation of Breast Masses".
- 1 2 "Breast Disorders: Breast Cancer". Merck Manual of Diagnosis and Therapy. February 2003. Archived from the original on 2 October 2011. Retrieved 5 February 2008.
- ↑ Watson M (2008). "Assessment of suspected cancer". InnoAiT. 1 (2): 94–107. doi:10.1093/innovait/inn001. S2CID 71908359.
- ↑ "Cancer Facts & Figures 2007" (PDF). American Cancer Society. 2007. Archived from the original (PDF) on 10 April 2007. Retrieved 26 April 2007.
- ↑ "Breast Cancer Evaluation". eMedicine. 23 August 2006. Archived from the original on 12 February 2008. Retrieved 5 February 2008.
- ↑ Ashikari R, Park K, Huvos AG, Urban JA (September 1970). "Paget's disease of the breast". Cancer. 26 (3): 680–5. doi:10.1002/1097-0142(197009)26:3<680::aid-cncr2820260329>3.0.co;2-p. PMID 4318756.
- ↑ Kollmorgen DR, Varanasi JS, Edge SB, Carson WE (August 1998). "Paget's disease of the breast: a 33-year experience". Journal of the American College of Surgeons. 187 (2): 171–7. doi:10.1016/S1072-7515(98)00143-4. PMID 9704964.
- ↑ Kleer CG, van Golen KL, Merajver SD (1 December 2000). "Molecular biology of breast cancer metastasis. Inflammatory breast cancer: clinical syndrome and molecular determinants". Breast Cancer Research. 2 (6): 423–9. doi:10.1186/bcr89. PMC 138665. PMID 11250736.
- 1 2 3 Gong P, Xia C, Yang Y, Lei W, Yang W, Yu J, Ji Y, Ren L, Ye F (July 2021). "Clinicopathologic profiling and oncologic outcomes of secretory carcinoma of the breast". Scientific Reports. 11 (1): 14738. Bibcode:2021NatSR..1114738G. doi:10.1038/s41598-021-94351-w. PMC 8289843. PMID 34282256.
- 1 2 Carretero-Barrio I, Santón A, Caniego Casas T, López Miranda E, Reguero-Callejas ME, Pérez-Mies B, Benito A, Palacios J (February 2022). "Cytological and molecular characterization of secretory breast carcinoma". Diagnostic Cytopathology. 50 (7): E174–E180. doi:10.1002/dc.24945. PMC 9303577. PMID 35156343. S2CID 246813006.
- ↑ Knaus ME, Grabowksi JE (August 2021). "Pediatric Breast Masses: An Overview of the Subtypes, Workup, Imaging, and Management". Advances in Pediatrics. 68: 195–209. doi:10.1016/j.yapd.2021.05.006. PMID 34243852. S2CID 235786044.
- ↑ Loo SK, Yates ME, Yang S, Oesterreich S, Lee AV, Wang XS (May 2022). "Fusion-associated carcinomas of the breast: Diagnostic, prognostic, and therapeutic significance". Genes, Chromosomes & Cancer. 61 (5): 261–273. doi:10.1002/gcc.23029. PMC 8930468. PMID 35106856.
- 1 2 Banerjee N, Banerjee D, Choudhary N (2021). "Secretory carcinoma of the breast, commonly exhibits the features of low grade, triple negative breast carcinoma- A Case report with updated review of literature". Autopsy & Case Reports. 11: e2020227. doi:10.4322/acr.2020.227. PMC 8101654. PMID 34277491.
- ↑ Li L, Wu N, Li F, Li L, Wei L, Liu J (February 2019). "Clinicopathologic and molecular characteristics of 44 patients with pure secretory breast carcinoma". Cancer Biology & Medicine. 16 (1): 139–146. doi:10.20892/j.issn.2095-3941.2018.0035. PMC 6528460. PMID 31119054.
- ↑ Mortensen L, Ordulu Z, Dagogo-Jack I, Bossuyt V, Winters L, Taghian A, Smith BL, Ellisen LW, Kiedrowski LA, Lennerz JK, Bardia A, Spring LM (October 2021). "Locally Recurrent Secretory Carcinoma of the Breast with NTRK3 Gene Fusion". The Oncologist. 26 (10): 818–824. doi:10.1002/onco.13880. PMC 8488779. PMID 34176200.
- ↑ answers.com. "Oncology Encyclopedia: Cystosarcoma Phyllodes". Answers.com. Archived from the original on 8 September 2010. Retrieved 10 August 2010.
- ↑ Lacroix M (December 2006). "Significance, detection and markers of disseminated breast cancer cells". Endocrine-Related Cancer. 13 (4): 1033–67. doi:10.1677/ERC-06-0001. PMID 17158753.
- ↑ "Stage 4 :: The National Breast Cancer Foundation". National Breast Cancer Foundation. Archived from the original on 1 February 2021. Retrieved 29 April 2019.
- ↑ National Cancer Institute (1 September 2004). "Metastatic Cancer: Questions and Answers". Archived from the original on 27 August 2008. Retrieved 6 February 2008.
- ↑ Perera N, Fernando N, Perera R (March 2020). "Metastatic breast cancer spread to peripancreatic lymph nodes causing biliary obstruction". The Breast Journal. 26 (3): 511–13. doi:10.1111/tbj.13531. PMID 31538691.
- ↑ Interpreting Signs and Symptoms. Lippincott Williams & Wilkins. 2007. pp. 99–. ISBN 978-1-58255-668-0.
- ↑ Merck Manual of Diagnosis and Therapy (February 2003). "Breast Disorders: Overview of Breast Disorders". Archived from the original on 3 October 2011. Retrieved 5 February 2008.
- 1 2 Hayes J, Richardson A, Frampton C (November 2013). "Population attributable risks for modifiable lifestyle factors and breast cancer in New Zealand women". Internal Medicine Journal. 43 (11): 1198–204. doi:10.1111/imj.12256. PMID 23910051. S2CID 23237732.
- ↑ Reeder JG, Vogel VG (2008). "Breast Cancer Prevention". Advances in Breast Cancer Management, Second Edition. Cancer Treatment and Research. Vol. 141. pp. 149–64. doi:10.1007/978-0-387-73161-2_10. ISBN 978-0-387-73160-5. PMID 18274088.
- 1 2 "Why we need to understand breast cancer risk". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 5 October 2023. doi:10.3310/nihrevidence_60242. S2CID 263690185. Archived from the original on 26 October 2023. Retrieved 26 October 2023.
- ↑ "Am I at risk?". Breast Cancer Care. 23 February 2018. Archived from the original on 25 October 2013. Retrieved 22 October 2013.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (July 2002). "Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease". Lancet. 360 (9328): 187–95. doi:10.1016/S0140-6736(02)09454-0. PMID 12133652. S2CID 25250519.
- ↑ Yager JD, Davidson NE (January 2006). "Estrogen carcinogenesis in breast cancer". The New England Journal of Medicine. 354 (3): 270–82. doi:10.1056/NEJMra050776. PMID 16421368. S2CID 5793142.
- ↑ Mazzucco A, Santoro E, DeSoto, M, Hong Lee J (February 2009). "Hormone Therapy and Menopause". National Research Center for Women & Families. Archived from the original on 7 August 2020. Retrieved 23 January 2018.
- ↑ Urbano T, Vinceti M, Wise LA, Filippini T (October 2021). "Light at night and risk of breast cancer: a systematic review and dose-response meta-analysis". International Journal of Health Geographics. 20 (1): 44. doi:10.1186/s12942-021-00297-7. PMC 8520294. PMID 34656111.
- 1 2 Zhang YB, Pan XF, Chen J, Cao A, Zhang YG, Xia L, et al. (March 2020). "Combined lifestyle factors, incident cancer, and cancer mortality: a systematic review and meta-analysis of prospective cohort studies". British Journal of Cancer. 122 (7): 1085–1093. doi:10.1038/s41416-020-0741-x. PMC 7109112. PMID 32037402.
- 1 2 Choi YJ, Myung SK, Lee JH (April 2018). "Light Alcohol Drinking and Risk of Cancer: A Meta-Analysis of Cohort Studies". Cancer Research and Treatment. 50 (2): 474–487. doi:10.4143/crt.2017.094. PMC 5912140. PMID 28546524.
- ↑ Bagnardi V, Rota M, Botteri E, Tramacere I, Islami F, Fedirko V, et al. (February 2015). "Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis". British Journal of Cancer. 112 (3): 580–593. doi:10.1038/bjc.2014.579. PMC 4453639. PMID 25422909.
- 1 2 Shield KD, Soerjomataram I, Rehm J (June 2016). "Alcohol Use and Breast Cancer: A Critical Review". Alcoholism: Clinical and Experimental Research. 40 (6): 1166–1181. doi:10.1111/acer.13071. PMID 27130687.
All levels of evidence showed a risk relationship between alcohol consumption and the risk of breast cancer, even at low levels of consumption.
- ↑ McDonald JA, Goyal A, Terry MB (September 2013). "Alcohol Intake and Breast Cancer Risk: Weighing the Overall Evidence". Current Breast Cancer Reports. 5 (3): 208–221. doi:10.1007/s12609-013-0114-z. PMC 3832299. PMID 24265860.
- ↑ Pearson-Stuttard J, Zhou B, Kontis V, Bentham J, Gunter MJ, Ezzati M (June 2018). "Worldwide burden of cancer attributable to diabetes and high body-mass index: a comparative risk assessment". The Lancet. Diabetes & Endocrinology. 6 (6): e6–e15. doi:10.1016/S2213-8587(18)30150-5. PMC 5982644. PMID 29803268.
- ↑ "Lifestyle-related Breast Cancer Risk Factors". www.cancer.org. Archived from the original on 27 July 2020. Retrieved 18 April 2018.
- ↑ Blackburn GL, Wang KA (September 2007). "Dietary fat reduction and breast cancer outcome: results from the Women's Intervention Nutrition Study (WINS)". The American Journal of Clinical Nutrition. 86 (3): s878-81. doi:10.1093/ajcn/86.3.878S. PMID 18265482.
- ↑ BBC report Weight link to breast cancer risk Archived 13 March 2007 at the Wayback Machine
- ↑ Kaiser J (November 2013). "Cancer. Cholesterol forges link between obesity and breast cancer". Science. 342 (6162): 1028. doi:10.1126/science.342.6162.1028. PMID 24288308.
- ↑ Aceves C, Anguiano B, Delgado G (April 2005). "Is iodine a gatekeeper of the integrity of the mammary gland?". Journal of Mammary Gland Biology and Neoplasia. 10 (2): 189–96. doi:10.1007/s10911-005-5401-5. PMID 16025225. S2CID 16838840.
- 1 2 Johnson KC, Miller AB, Collishaw NE, Palmer JR, Hammond SK, Salmon AG, et al. (January 2011). "Active smoking and secondhand smoke increase breast cancer risk: the report of the Canadian Expert Panel on Tobacco Smoke and Breast Cancer Risk (2009)". Tobacco Control. 20 (1): e2. doi:10.1136/tc.2010.035931. PMID 21148114. S2CID 448229.
- ↑ Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT (July 2012). "Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy". Lancet. 380 (9838): 219–29. doi:10.1016/S0140-6736(12)61031-9. PMC 3645500. PMID 22818936.
- ↑ Biswas A, Oh PI, Faulkner GE, Bajaj RR, Silver MA, Mitchell MS, Alter DA (January 2015). "Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis". Annals of Internal Medicine. 162 (2): 123–32. doi:10.7326/M14-1651. PMID 25599350. S2CID 7256176.
- ↑ Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. (December 2015). "Breastfeeding and maternal health outcomes: a systematic review and meta-analysis". Acta Paediatrica. 104 (467): 96–113. doi:10.1111/apa.13102. PMC 4670483. PMID 26172878.
- ↑ "Breastfeeding". World Health Organization. Archived from the original on 29 May 2019. Retrieved 18 November 2021.
- ↑ "Breastfeeding:Frequently Asked Questions (FAQs)". U.S. Center for disease control and prevention(CDC). 10 August 2021. Archived from the original on 6 May 2019. Retrieved 18 November 2021.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (July 2002). "Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease". Lancet. 360 (9328): 187–195. doi:10.1016/S0140-6736(02)09454-0. PMID 12133652. S2CID 25250519.
- ↑ Russo J, Russo IH (August 1980). "Susceptibility of the mammary gland to carcinogenesis. II. Pregnancy interruption as a risk factor in tumor incidence". The American Journal of Pathology. 100 (2): 497–512. PMC 1903536. PMID 6773421.
In contrast, abortion is associated with increased risk of carcinomas of the breast. The explanation for these epidemiologic findings is not known, but the parallelism between the DMBA-induced rat mammary carcinoma model and the human situation is striking. ... Abortion would interrupt this process, leaving in the gland undifferentiated structures like those observed in the rat mammary gland, which could render the gland again susceptible to carcinogenesis.
- ↑ Beral V, Bull D, Doll R, Peto R, Reeves G (March 2004). "Breast cancer and abortion: collaborative reanalysis of data from 53 epidemiological studies, including 83?000 women with breast cancer from 16 countries". Lancet. 363 (9414): 1007–16. doi:10.1016/S0140-6736(04)15835-2. PMID 15051280. S2CID 20751083.
- 1 2 American Cancer Society (2005). "Breast Cancer Facts & Figures 2005–2006" (PDF). Archived from the original (PDF) on 13 June 2007. Retrieved 26 April 2007.
- ↑ Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC (March 2011). "Shift work and chronic disease: the epidemiological evidence". Occupational Medicine. 61 (2): 78–89. doi:10.1093/occmed/kqr001. PMC 3045028. PMID 21355031.
- ↑ Marinac CR, Nelson SH, Breen CI, Hartman SJ, Natarajan L, Pierce JP, et al. (August 2016). "Prolonged Nightly Fasting and Breast Cancer Prognosis". JAMA Oncology. 2 (8): 1049–55. doi:10.1001/jamaoncol.2016.0164. PMC 4982776. PMID 27032109.
- ↑ Brody JG, Rudel RA, Michels KB, Moysich KB, Bernstein L, Attfield KR, Gray S (June 2007). "Environmental pollutants, diet, physical activity, body size, and breast cancer: where do we stand in research to identify opportunities for prevention?". Cancer. 109 (12 Suppl): 2627–34. doi:10.1002/cncr.22656. PMID 17503444. S2CID 34880415.
- ↑ Hendrick RE (October 2010). "Radiation doses and cancer risks from breast imaging studies". Radiology. 257 (1): 246–53. doi:10.1148/radiol.10100570. PMID 20736332.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (September 2019). "Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence". Lancet. 394 (10204): 1159–1168. doi:10.1016/S0140-6736(19)31709-X. PMC 6891893. PMID 31474332.
- 1 2 "Risk of breast cancer with HRT depends on therapy type and duration". NIHR Evidence. National Institute for Health and Care Research. 20 December 2021. doi:10.3310/alert_48575. Archived from the original on 26 October 2023. Retrieved 26 October 2023.
- 1 2 Vinogradova Y, Coupland C, Hippisley-Cox J (October 2020). "Use of hormone replacement therapy and risk of breast cancer: nested case-control studies using the QResearch and CPRD databases". BMJ. 371: m3873. doi:10.1136/bmj.m3873. PMC 7592147. PMID 33115755.
- ↑ Kanadys W, Barańska A, Malm M, Błaszczuk A, Polz-Dacewicz M, Janiszewska M, Jędrych M (April 2021). "Use of Oral Contraceptives as a Potential Risk Factor for Breast Cancer: A Systematic Review and Meta-Analysis of Case-Control Studies Up to 2010". International Journal of Environmental Research and Public Health. 18 (9): 4638. doi:10.3390/ijerph18094638. PMC 8123798. PMID 33925599.
- 1 2 Chelmow D, Pearlman MD, Young A, Bozzuto L, Dayaratna S, Jeudy M, et al. (June 2020). "Executive Summary of the Early-Onset Breast Cancer Evidence Review Conference". Obstetrics and Gynecology. 135 (6): 1457–1478. doi:10.1097/AOG.0000000000003889. PMC 7253192. PMID 32459439.
- ↑ Gaffield ME, Culwell KR, Ravi A (October 2009). "Oral contraceptives and family history of breast cancer". Contraception. 80 (4): 372–380. doi:10.1016/j.contraception.2009.04.010. PMID 19751860.
- ↑ Huber D, Seitz S, Kast K, Emons G, Ortmann O (April 2020). "Use of oral contraceptives in BRCA mutation carriers and risk for ovarian and breast cancer: a systematic review". Archives of Gynecology and Obstetrics. 301 (4): 875–884. doi:10.1007/s00404-020-05458-w. PMC 8494665. PMID 32140806.
- 1 2 3 Gage M, Wattendorf D, Henry LR (April 2012). "Translational advances regarding hereditary breast cancer syndromes". Journal of Surgical Oncology. 105 (5): 444–51. doi:10.1002/jso.21856. PMID 22441895. S2CID 3406636.
- ↑ Colditz GA, Kaphingst KA, Hankinson SE, Rosner B (June 2012). "Family history and risk of breast cancer: nurses' health study". Breast Cancer Research and Treatment. 133 (3): 1097–104. doi:10.1007/s10549-012-1985-9. PMC 3387322. PMID 22350789.
- ↑ Collaborative Group on Hormonal Factors in Breast Cancer (October 2001). "Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease". Lancet. 358 (9291): 1389–99. doi:10.1016/S0140-6736(01)06524-2. PMID 11705483. S2CID 24278814.
- ↑ Nelson HD, Zakher B, Cantor A, Fu R, Griffin J, O'Meara ES, et al. (May 2012). "Risk factors for breast cancer for women aged 40 to 49 years: a systematic review and meta-analysis". Annals of Internal Medicine. 156 (9): 635–48. doi:10.7326/0003-4819-156-9-201205010-00006. PMC 3561467. PMID 22547473.
- 1 2 Pasche B (2010). Cancer Genetics (Cancer Treatment and Research). Berlin: Springer. pp. 19–20. ISBN 978-1-4419-6032-0.
- ↑ Kolata G (23 September 2012). "Genetic Study Finds 4 Distinct Variations of Breast Cancer". The New York Times. Archived from the original on 24 September 2012. Retrieved 23 September 2012.
- ↑ "CDC – What Are the Risk Factors for Breast Cancer?". www.cdc.gov. 14 December 2018. Archived from the original on 13 August 2020. Retrieved 29 April 2019.
- ↑ Tian JM, Ran B, Zhang CL, Yan DM, Li XH (January 2018). "Estrogen and progesterone promote breast cancer cell proliferation by inducing cyclin G1 expression". Brazilian Journal of Medical and Biological Research. 51 (3): 1–7. doi:10.1590/1414-431X20175612. PMC 5912097. PMID 29513878. Archived from the original on 14 May 2017. Retrieved 29 April 2019.
- ↑ "Understanding Breast Changes – National Cancer Institute". Archived from the original on 27 May 2010.
- ↑ "Breast Cancer Treatment". National Cancer Institute. January 1980. Archived from the original on 25 April 2015.
- ↑ Afonso N, Bouwman D (August 2008). "Lobular carcinoma in situ". European Journal of Cancer Prevention. 17 (4): 312–6. doi:10.1097/CEJ.0b013e3282f75e5d. PMID 18562954. S2CID 388045.
- ↑ Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, et al. (September 2013). "Risk factors of breast cancer: a systematic review and meta-analysis". Asia-Pacific Journal of Public Health. 25 (5): 368–87. doi:10.1177/1010539513488795. PMID 23709491. S2CID 206616972.
- ↑ Böhm I (June 2011). "Breast cancer in lupus". Breast. 20 (3): 288–90. doi:10.1016/j.breast.2010.12.005. PMID 21237645.
- ↑ Williams C, Lin CY (November 2013). "Oestrogen receptors in breast cancer: basic mechanisms and clinical implications". ecancermedicalscience. 7: 370. doi:10.3332/ecancer.2013.370. PMC 3816846. PMID 24222786.
- ↑ Levin ER, Pietras RJ (April 2008). "Estrogen receptors outside the nucleus in breast cancer". Breast Cancer Research and Treatment. 108 (3): 351–361. doi:10.1007/s10549-007-9618-4. PMID 17592774. S2CID 11394158.
- ↑ Wang M, Wu X, Chai F, Zhang Y, Jiang J (May 2016). "Plasma prolactin and breast cancer risk: a meta- analysis". Scientific Reports. 6: 25998. Bibcode:2016NatSR...625998W. doi:10.1038/srep25998. PMC 4869065. PMID 27184120.
- ↑ Leung JC, Ng DW, Chu RY, Chan EW, Huang L, Lum DH, et al. (September 2022). "Association of antipsychotic use with breast cancer: a systematic review and meta-analysis of observational studies with over 2 million individuals". Epidemiology and Psychiatric Sciences. 31: e61. doi:10.1017/S2045796022000476. PMC 9483823. PMID 36059215.
- ↑ Lee A, Arteaga C (14 December 2009). "32nd Annual CTRC-AACR San Antonio Breast Cancer Symposium" (PDF). Sunday Morning Year-End Review. Archived from the original (PDF) on 13 August 2013.
- ↑ Cavalieri E, Chakravarti D, Guttenplan J, Hart E, Ingle J, Jankowiak R, et al. (August 2006). "Catechol estrogen quinones as initiators of breast and other human cancers: implications for biomarkers of susceptibility and cancer prevention". Biochimica et Biophysica Acta (BBA) - Reviews on Cancer. 1766 (1): 63–78. doi:10.1016/j.bbcan.2006.03.001. PMID 16675129.
- ↑ Filardo EJ (February 2018). "A role for G-protein coupled estrogen receptor (GPER) in estrogen-induced carcinogenesis: Dysregulated glandular homeostasis, survival and metastasis". The Journal of Steroid Biochemistry and Molecular Biology. 176: 38–48. doi:10.1016/j.jsbmb.2017.05.005. PMID 28595943. S2CID 19644829.
- ↑ Haslam SZ, Woodward TL (June 2003). "Host microenvironment in breast cancer development: epithelial-cell-stromal-cell interactions and steroid hormone action in normal and cancerous mammary gland". Breast Cancer Research. 5 (4): 208–15. doi:10.1186/bcr615. PMC 165024. PMID 12817994.
- ↑ Wiseman BS, Werb Z (May 2002). "Stromal effects on mammary gland development and breast cancer". Science. 296 (5570): 1046–9. Bibcode:2002Sci...296.1046W. doi:10.1126/science.1067431. PMC 2788989. PMID 12004111.
- ↑ Jardé T, Perrier S, Vasson MP, Caldefie-Chézet F (January 2011). "Molecular mechanisms of leptin and adiponectin in breast cancer". European Journal of Cancer. 47 (1): 33–43. doi:10.1016/j.ejca.2010.09.005. PMID 20889333.
- ↑ Dunning AM, Healey CS, Pharoah PD, Teare MD, Ponder BA, Easton DF (October 1999). "A systematic review of genetic polymorphisms and breast cancer risk". Cancer Epidemiology, Biomarkers & Prevention. 8 (10): 843–54. PMID 10548311. Archived from the original on 7 July 2012. Retrieved 26 June 2009.
- ↑ Begg CB, Haile RW, Borg A, Malone KE, Concannon P, Thomas DC, et al. (January 2008). "Variation of breast cancer risk among BRCA1/2 carriers". JAMA. 299 (2): 194–201. doi:10.1001/jama.2007.55-a. PMC 2714486. PMID 18182601.
- ↑ Patel KJ, Yu VP, Lee H, Corcoran A, Thistlethwaite FC, Evans MJ, et al. (February 1998). "Involvement of Brca2 in DNA repair". Molecular Cell. 1 (3): 347–57. doi:10.1016/S1097-2765(00)80035-0. PMID 9660919.
- ↑ Marietta C, Thompson LH, Lamerdin JE, Brooks PJ (May 2009). "Acetaldehyde stimulates FANCD2 monoubiquitination, H2AX phosphorylation, and BRCA1 phosphorylation in human cells in vitro: implications for alcohol-related carcinogenesis". Mutation Research. 664 (1–2): 77–83. doi:10.1016/j.mrfmmm.2009.03.011. PMC 2807731. PMID 19428384.
- ↑ Theruvathu JA, Jaruga P, Nath RG, Dizdaroglu M, Brooks PJ (2005). "Polyamines stimulate the formation of mutagenic 1,N2-propanodeoxyguanosine adducts from acetaldehyde". Nucleic Acids Research. 33 (11): 3513–20. doi:10.1093/nar/gki661. PMC 1156964. PMID 15972793.
- ↑ Wooster R, Weber BL (June 2003). "Breast and ovarian cancer". The New England Journal of Medicine. 348 (23): 2339–47. doi:10.1056/NEJMra012284. PMID 12788999. S2CID 26602401.
- ↑ Levin B, Lech D, Friedenson B (December 2012). "Evidence that BRCA1- or BRCA2-associated cancers are not inevitable". Molecular Medicine. 18 (9): 1327–37. doi:10.2119/molmed.2012.00280. PMC 3521784. PMID 22972572.
- ↑ Polansky H, Schwab H (August 2019). "How latent viruses cause breast cancer: An explanation based on the microcompetition model". Bosnian Journal of Basic Medical Sciences. 19 (3): 221–226. doi:10.17305/bjbms.2018.3950. PMC 6716096. PMID 30579323.
- ↑ Kouros-Mehr H, Kim JW, Bechis SK, Werb Z (April 2008). "GATA-3 and the regulation of the mammary luminal cell fate". Current Opinion in Cell Biology. 20 (2): 164–70. doi:10.1016/j.ceb.2008.02.003. PMC 2397451. PMID 18358709.
- 1 2 "Breast Cancer Screening PDQ – Patient Version". National Cancer Institute. 26 June 2023. Retrieved 5 January 2024.
- ↑ "Findings on a Mammogram and Mammogram Results". Susan G. Komen Foundation. 30 November 2022. Retrieved 5 January 2024.
- ↑ Nielsen & Narayan 2023, "Interpretation of a Mammogram".
- ↑ Metaxa, Healy & O'Keeffe 2019, "Introduction".
- ↑ "Understanding Your Mammogram Report". American Cancer Society. 14 January 2022. Retrieved 8 January 2024.
- ↑ "Breast Density and Your Mammogram Report". American Cancer Society. 28 March 2023. Retrieved 8 January 2024.
- ↑ Nielsen & Narayan 2023, "Implications of Breast Density".
- 1 2 Harbeck et al. 2019, "Screening".
- ↑ Loibl et al. 2021, "Screening".
- 1 2 Hayes & Lippman 2022, "Screening for Breast Cancer".
- ↑ Rahman & Helvie 2022, "Table 1".
- ↑ "Breast Cancer Screening (PDQ) - Health Professional Version". National Cancer Institute. 7 June 2023. Retrieved 10 January 2024.
- ↑ Menes et al. 2021, "Abstract".
- ↑ Qaseem A, Lin JS, Mustafa RA, Horwitch CA, Wilt TJ (April 2019). "Screening for Breast Cancer in Average-Risk Women: A Guidance Statement From the American College of Physicians". Annals of Internal Medicine. 170 (8): 547–560. doi:10.7326/M18-2147. PMID 30959525.
- ↑ Biesheuvel C, Weigel S, Heindel W (2011). "Mammography Screening: Evidence, History and Current Practice in Germany and Other European Countries". Breast Care. 6 (2): 104–109. doi:10.1159/000327493. PMC 3104900. PMID 21673820.
- ↑ Schünemann HJ, Lerda D, Quinn C, Follmann M, Alonso-Coello P, Rossi PG, et al. (January 2020). "Breast Cancer Screening and Diagnosis: A Synopsis of the European Breast Guidelines". Annals of Internal Medicine. 172 (1): 46–56. doi:10.7326/M19-2125. PMID 31766052.
- ↑ Tonelli M, Connor Gorber S, Joffres M, Dickinson J, Singh H, Lewin G, et al. (November 2011). "Recommendations on screening for breast cancer in average-risk women aged 40–74 years". CMAJ. 183 (17): 1991–2001. doi:10.1503/cmaj.110334. PMC 3225421. PMID 22106103.
- ↑ Moss S (August 2004). "Should women under 50 be screened for breast cancer?". British Journal of Cancer. 91 (3): 413–417. doi:10.1038/sj.bjc.6601966. PMC 2409834. PMID 15213718.
- ↑ "Breast Cancer: Screening". United States Preventive Services Task Force. Archived from the original on 16 June 2013.
- 1 2 "Breast Biopsy". National Breast Cancer Foundation. Retrieved 10 January 2024.
- ↑ Harbeck et al. 2019, "Diagnostic Work-Up".
- ↑ Hayes & Lippman 2022, "Pathologic Findings of the Breast".
- ↑ Kosir MA (July 2019). "Ch. 253, Breast Cancer". Merck Manual, Professional Edition. Archived from the original on 10 November 2011.
- ↑ American Society of Clinical Oncology, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American Society of Clinical Oncology, archived from the original (PDF) on 31 July 2012, retrieved 14 August 2012
- ↑ Carlson RW, Allred DC, Anderson BO, Burstein HJ, Carter WB, Edge SB, et al. (February 2009). "Breast cancer. Clinical practice guidelines in oncology". Journal of the National Comprehensive Cancer Network. 7 (2): 122–92. doi:10.6004/jnccn.2009.0012. PMID 19200416.
- ↑ Kumar V, Abbas A (2010). Robbins and Cotran Pathologic Basis of Disease. Philadelphia: Saunders, an imprint of Elsevier inc. p. 1090. ISBN 978-1-4160-3121-5.
- ↑ Sotiriou C, Pusztai L (February 2009). "Gene-expression signatures in breast cancer". The New England Journal of Medicine. 360 (8): 790–800. doi:10.1056/NEJMra0801289. PMID 19228622.
- ↑ Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE, Davidson NE, et al. (October 2005). "Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer". The New England Journal of Medicine. 353 (16): 1673–84. doi:10.1056/NEJMoa052122. PMID 16236738. S2CID 9534884.
- 1 2 3 "Lifestyle-related Breast Cancer Risk Factors". www.cancer.org. Archived from the original on 27 July 2020. Retrieved 18 April 2018.
- ↑ Eliassen AH, Hankinson SE, Rosner B, Holmes MD, Willett WC (October 2010). "Physical activity and risk of breast cancer among postmenopausal women". Archives of Internal Medicine. 170 (19): 1758–64. doi:10.1001/archinternmed.2010.363. PMC 3142573. PMID 20975025.
- ↑ Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. (August 2016). "Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013". BMJ. 354: i3857. doi:10.1136/bmj.i3857. PMC 4979358. PMID 27510511.
- ↑ "New study finds 'strong evidence' that exercise cuts breast cancer risk". belfasttelegraph. ISSN 0307-1235. Archived from the original on 7 September 2022. Retrieved 7 September 2022.
- ↑ Runowicz CD, Leach CR, Henry NL, Henry KS, Mackey HT, Cowens-Alvarado RL, et al. (January 2016). "American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline". CA: A Cancer Journal for Clinicians. 66 (1): 43–73. doi:10.3322/caac.21319. hdl:2027.42/136493. PMID 26641959.
- ↑ Farvid MS, Spence ND, Holmes MD, Barnett JB (July 2020). "Fiber consumption and breast cancer incidence: A systematic review and meta-analysis of prospective studies". Cancer. 126 (13): 3061–3075. doi:10.1002/cncr.32816. PMID 32249416. S2CID 214809009.
- ↑ Farvid MS, Barnett JB, Spence ND (July 2021). "Fruit and vegetable consumption and incident breast cancer: a systematic review and meta-analysis of prospective studies". British Journal of Cancer. 125 (2): 284–298. doi:10.1038/s41416-021-01373-2. PMC 8292326. PMID 34006925.
- ↑ Song JK, Bae JM (March 2013). "Citrus fruit intake and breast cancer risk: a quantitative systematic review". Journal of Breast Cancer. 16 (1): 72–6. doi:10.4048/jbc.2013.16.1.72. PMC 3625773. PMID 23593085.
- ↑ Zheng JS, Hu XJ, Zhao YM, Yang J, Li D (June 2013). "Intake of fish and marine n-3 polyunsaturated fatty acids and risk of breast cancer: meta-analysis of data from 21 independent prospective cohort studies". BMJ. 346: f3706. doi:10.1136/bmj.f3706. PMID 23814120.
- ↑ Wu AH, Yu MC, Tseng CC, Pike MC (January 2008). "Epidemiology of soy exposures and breast cancer risk". British Journal of Cancer. 98 (1): 9–14. doi:10.1038/sj.bjc.6604145. PMC 2359677. PMID 18182974.
- ↑ Hartmann LC, Schaid DJ, Woods JE, Crotty TP, Myers JL, Arnold PG, et al. (January 1999). "Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer". The New England Journal of Medicine. 340 (2): 77–84. doi:10.1056/NEJM199901143400201. PMID 9887158.
- ↑ Meijers-Heijboer H, van Geel B, van Putten WL, Henzen-Logmans SC, Seynaeve C, Menke-Pluymers MB, et al. (July 2001). "Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation" (PDF). The New England Journal of Medicine. 345 (3): 159–64. doi:10.1056/NEJM200107193450301. PMID 11463009. Archived (PDF) from the original on 20 June 2022. Retrieved 10 May 2022.
- 1 2 Carbine NE, Lostumbo L, Wallace J, Ko H (April 2018). "Risk-reducing mastectomy for the prevention of primary breast cancer". The Cochrane Database of Systematic Reviews. 4 (4): CD002748. doi:10.1002/14651858.cd002748.pub4. PMC 6494635. PMID 29620792.
- 1 2 Moyer VA (February 2014). "Risk assessment, genetic counseling, and genetic testing for BRCA-related cancer in women: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 160 (4): 271–81. doi:10.7326/M13-2747. PMID 24366376.
- ↑ "Earlier decisions on breast and ovarian surgery reduce cancer in women at high risk". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 7 December 2021. doi:10.3310/alert_48318. S2CID 263487127. Archived from the original on 27 June 2022. Retrieved 21 December 2022.
- ↑ Marcinkute R, Woodward ER, Gandhi A, Howell S, Crosbie EJ, Wissely J, et al. (February 2022). "Uptake and efficacy of bilateral risk reducing surgery in unaffected female BRCA1 and BRCA2 carriers". Journal of Medical Genetics. 59 (2): 133–140. doi:10.1136/jmedgenet-2020-107356. PMID 33568438. S2CID 231876899. Archived from the original on 2 February 2023. Retrieved 21 December 2022.
- 1 2 Nelson HD, Smith ME, Griffin JC, Fu R (April 2013). "Use of medications to reduce risk for primary breast cancer: a systematic review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 158 (8): 604–14. doi:10.7326/0003-4819-158-8-201304160-00005. PMID 23588749.
- ↑ Cuzick J, Sestak I, Bonanni B, Costantino JP, Cummings S, DeCensi A, et al. (May 2013). "Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data". Lancet. 381 (9880): 1827–34. doi:10.1016/S0140-6736(13)60140-3. PMC 3671272. PMID 23639488.
- ↑ Owens DK, Davidson KW, Krist AH, Barry MJ, Cabana M, Caughey AB, et al. (September 2019). "Medication Use to Reduce Risk of Breast Cancer: US Preventive Services Task Force Recommendation Statement". JAMA. 322 (9): 857–867. doi:10.1001/jama.2019.11885. PMID 31479144.
- ↑ Cuzick J, Sestak I, Bonanni B, Costantino JP, Cummings S, DeCensi A, et al. (May 2013). "Selective oestrogen receptor modulators in prevention of breast cancer: an updated meta-analysis of individual participant data". Lancet. 381 (9880): 1827–34. doi:10.1016/S0140-6736(13)60140-3. PMC 3671272. PMID 23639488.
- ↑ Mocellin S, Goodwin A, Pasquali S (April 2019). "Risk-reducing medications for primary breast cancer: a network meta-analysis". The Cochrane Database of Systematic Reviews. 2019 (4): CD012191. doi:10.1002/14651858.cd012191.pub2. PMC 6487387. PMID 31032883.
- ↑ Saini KS, Taylor C, Ramirez AJ, Palmieri C, Gunnarsson U, Schmoll HJ, et al. (April 2012). "Role of the multidisciplinary team in breast cancer management: results from a large international survey involving 39 countries". Annals of Oncology. 23 (4): 853–9. doi:10.1093/annonc/mdr352. PMID 21821551.
- ↑ Khalil DN, Smith EL, Brentjens RJ, Wolchok JD (May 2016). "The future of cancer treatment: immunomodulation, CARs and combination immunotherapy". Nature Reviews. Clinical Oncology. 13 (5): 273–90. doi:10.1038/nrclinonc.2016.25. PMC 5551685. PMID 26977780.
- ↑ Leite AM, Macedo AV, Jorge AJ, Martins WA (August 2018). "Antiplatelet Therapy in Breast Cancer Patients Using Hormonal Therapy: Myths, Evidence and Potentialities – Systematic Review". Arquivos Brasileiros de Cardiologia. 111 (2): 205–212. doi:10.5935/abc.20180138. PMC 6122903. PMID 30183988.
- ↑ Holmes MD, Chen WY, Li L, Hertzmark E, Spiegelman D, Hankinson SE (March 2010). "Aspirin intake and survival after breast cancer". Journal of Clinical Oncology. 28 (9): 1467–72. doi:10.1200/JCO.2009.22.7918. PMC 2849768. PMID 20159825.
- ↑ Bao T, Rudek MA (2011). "The Clinical Pharmacology of Anastrozole". European Oncology & Haematology. 7 (2): 106–8. doi:10.17925/EOH.2011.07.02.106. S2CID 1802863.
- ↑ Burstein HJ, Temin S, Anderson H, Buchholz TA, Davidson NE, Gelmon KE, et al. (July 2014). "Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: american society of clinical oncology clinical practice guideline focused update". Journal of Clinical Oncology. 32 (21): 2255–69. doi:10.1200/JCO.2013.54.2258. PMC 4876310. PMID 24868023.
- ↑ Romero SA, Young K, Hickey M, Su HI (21 December 2020). "Levonorgestrel intrauterine system for endometrial protection in women with breast cancer on adjuvant tamoxifen". Cochrane Database Syst Rev. 12 (2): CD007245. doi:10.1002/14651858.CD007245.pub4. PMC 8092675. PMID 33348436.
- ↑ Early Breast Cancer Trialists' Collaborative Group (EBCTCG) (October 2015). "Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials". Lancet. 386 (10001): 1341–1352. doi:10.1016/S0140-6736(15)61074-1. hdl:10044/1/32438. PMID 26211827.
- ↑ Petit T, Dufour P, Tannock I (June 2011). "A critical evaluation of the role of aromatase inhibitors as adjuvant therapy for postmenopausal women with breast cancer". Endocrine-Related Cancer. 18 (3): R79-89. doi:10.1530/ERC-10-0162. PMID 21502311.
- ↑ "Treatment of metastatic breast cancer". www.uptodate.com. Archived from the original on 4 September 2017. Retrieved 4 September 2017.
- ↑ "Combination of Ribociclib and Letrozole Is a Home Run in Advanced Breast Cancer – The ASCO Post". ascopost.com. Archived from the original on 29 July 2020. Retrieved 31 January 2019.
- ↑ Jahanzeb M (August 2008). "Adjuvant trastuzumab therapy for HER2-positive breast cancer". Clinical Breast Cancer. 8 (4): 324–33. doi:10.3816/CBC.2008.n.037. PMID 18757259.
- ↑ "Entrez Gene: ERBB2 v-erb-b2 erythroblastic leukemia viral oncogene homolog 2, neuro/glioblastoma derived oncogene homolog (avian)". Archived from the original on 26 October 2009. Retrieved 17 November 2015.
- ↑ "Herceptin (trastuzumab) Adjuvant HER2+ Breast Cancer Therapy Pivotal Studies and Efficacy Data". Herceptin.com. Archived from the original on 6 April 2010. Retrieved 8 May 2010.
- ↑ "New ASCO Guidelines on Treating Advanced-Stage HER2-Positive Breast Cancer". Breastcancer.org. 4 October 2016. Archived from the original on 27 July 2020. Retrieved 31 January 2019.
- ↑ Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. (March 2001). "Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2". The New England Journal of Medicine. 344 (11): 783–92. doi:10.1056/NEJM200103153441101. PMID 11248153.
- ↑ "FDA approves elacestrant for ER-positive, HER2-negative, ESR1-mutated advanced or metastatic breast cancer". U.S. Food and Drug Administration (FDA). 27 January 2023. Archived from the original on 2 February 2023. Retrieved 1 February 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Stemline Therapeutics Inc., a wholly owned subsidiary of Menarini Group, Receives Approval from U.S. FDA for Orserdu (elacestrant) as the First and Only Treatment Specifically Indicated for Patients with ESR1 Mutations in ER+, HER2- Advanced or Metastatic Breast Cancer". Radius (Press release). 31 January 2023. Archived from the original on 2 February 2023. Retrieved 1 February 2023.
- ↑ "FDA approves capivasertib with fulvestrant for breast cancer". U.S. Food and Drug Administration. 16 November 2023. Archived from the original on 17 November 2023. Retrieved 17 November 2023.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - ↑ "Oncology (Cancer) / Hematologic Malignancies Approval Notifications". U.S. Food and Drug Administration. 16 November 2023. Archived from the original on 17 November 2023. Retrieved 17 November 2023.
- ↑ "Truqap (capivasertib) plus Faslodex approved in the US for patients with advanced HR-positive breast cancer". AstraZeneca (Press release). 17 November 2023. Archived from the original on 17 November 2023. Retrieved 17 November 2023.
- ↑ Massarut S, Baldassare G, Belleti B, Reccanello S, D'Andrea S, Ezio C, Perin T, Roncadin M, Vaidya JS (2006). "Intraoperative radiotherapy impairs breast cancer cell motility induced by surgical wound fluid". J Clin Oncol. 24 (18S): 10611. doi:10.1200/jco.2006.24.18_suppl.10611. Archived from the original on 12 January 2012. Retrieved 9 June 2010.
- ↑ Belletti B, Vaidya JS, D'Andrea S, Entschladen F, Roncadin M, Lovat F, et al. (March 2008). "Targeted intraoperative radiotherapy impairs the stimulation of breast cancer cell proliferation and invasion caused by surgical wounding". Clinical Cancer Research. 14 (5): 1325–32. doi:10.1158/1078-0432.CCR-07-4453. PMID 18316551.
- ↑ "Radiation Therapy". Breastcancer.org. Archived from the original on 17 November 2015. Retrieved 17 November 2015.
- ↑ Hickey BE, Lehman M (30 August 2021). "Partial breast irradiation versus whole breast radiotherapy for early breast cancer". The Cochrane Database of Systematic Reviews. 2021 (8): CD007077. doi:10.1002/14651858.CD007077.pub4. PMC 8406917. PMID 34459500.
- ↑ Moschetti I, Cinquini M, Lambertini M, Levaggi A, Liberati A (May 2016). "Follow-up strategies for women treated for early breast cancer". The Cochrane Database of Systematic Reviews. 2016 (5): CD001768. doi:10.1002/14651858.cd001768.pub3. PMC 7073405. PMID 27230946.
- ↑ Khan F, Amatya B, Ng L, Demetrios M, Zhang NY, Turner-Stokes L (December 2012). "Multidisciplinary rehabilitation for follow-up of women treated for breast cancer". The Cochrane Database of Systematic Reviews. 12 (3): CD009553. doi:10.1002/14651858.cd009553.pub2. PMC 8078577. PMID 23235677.
- ↑ Lee TS, Kilbreath SL, Refshauge KM, Herbert RD, Beith JM (July 2008). "Prognosis of the upper limb following surgery and radiation for breast cancer". Breast Cancer Research and Treatment. 110 (1): 19–37. doi:10.1007/s10549-007-9710-9. PMID 17899373. S2CID 24976113.
- ↑ "Exercise programme improves arm function and pain after breast cancer surgery". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 26 September 2022. doi:10.3310/nihrevidence_53632. S2CID 252562000. Archived from the original on 28 September 2022. Retrieved 28 September 2022.
- ↑ Bruce J, Mazuquin B, Mistry P, Rees S, Canaway A, Hossain A, et al. (February 2022). "Exercise to prevent shoulder problems after breast cancer surgery: the PROSPER RCT". Health Technology Assessment. 26 (15): 1–124. doi:10.3310/JKNZ2003. PMID 35220995. S2CID 247157545.
- ↑ Data from Mangone L, Marinelli F, Bisceglia I, Braghiroli MB, Damato A, Pinto C (2022). "Five-year relative survival by stage of breast and colon cancers in northern Italy". Front Oncol. 12: 982461. doi:10.3389/fonc.2022.982461. PMC 9659859. PMID 36387150.
- ↑ "Surgery Choices for Women with Early Stage Breast Cancer" (PDF). National Cancer Institute and the National Research Center for Women & Families. August 2004. Archived from the original (PDF) on 13 August 2013.
- ↑ Elston CW, Ellis IO (November 1991). "Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up". Histopathology. 19 (5): 403–10. doi:10.1111/j.1365-2559.1991.tb00229.x. PMID 1757079. S2CID 17622089.
- ↑ Peppercorn J (2009). "Breast Cancer in Women Under 40". Oncology. 23 (6): 465–74. PMID 19544685. Archived from the original on 16 June 2009.
- ↑ Pritchard KI (2009). "Ovarian Suppression/Ablation in Premenopausal ER-Positive Breast Cancer Patients". Oncology. 23 (1). Archived from the original on 5 July 2009.
- ↑ Jassim GA, Doherty S, Whitford DL, Khashan AS (January 2023). "Psychological interventions for women with non-metastatic breast cancer". The Cochrane Database of Systematic Reviews. 2023 (1): CD008729. doi:10.1002/14651858.CD008729.pub3. PMC 9832339. PMID 36628983.
- ↑ Lahart IM, Metsios GS, Nevill AM, Carmichael AR (January 2018). "Physical activity for women with breast cancer after adjuvant therapy". The Cochrane Database of Systematic Reviews. 1 (1): CD011292. doi:10.1002/14651858.cd011292.pub2. PMC 6491330. PMID 29376559.
- ↑ de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE, et al. (April 2013). "Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care". Cancer Epidemiology, Biomarkers & Prevention. 22 (4): 561–570. doi:10.1158/1055-9965.EPI-12-1356. PMC 3654837. PMID 23535024.
- ↑ Siegel RL, Miller KD, Fuchs HE, Jemal A (January 2022). "Cancer statistics, 2022". CA. 72 (1): 7–33. doi:10.3322/caac.21708. PMID 35020204. S2CID 245878846.
- ↑ Raisi-Estabragh Z, Kobo O, Freeman P, Petersen SE, Kolman L, Miller RJ, et al. (December 2022). "Temporal trends in disease-specific causes of cardiovascular mortality amongst patients with cancer in the USA between 1999 and 2019". European Heart Journal. Quality of Care & Clinical Outcomes. 9 (1): 54–63. doi:10.1093/ehjqcco/qcac016. PMC 9745666. PMID 35435219.
- 1 2 3 4 Galimzhanov A, Istanbuly S, Tun HN, Ozbay B, Alasnag M, Ky B, et al. (July 2023). "Cardiovascular outcomes in breast cancer survivors: a systematic review and meta-analysis". European Journal of Preventive Cardiology. 30 (18): 2018–2031. doi:10.1093/eurjpc/zwad243. PMID 37499186.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- 1 2 McGuire A, Brown JA, Malone C, McLaughlin R, Kerin MJ (May 2015). "Effects of age on the detection and management of breast cancer". Cancers. 7 (2): 908–29. doi:10.3390/cancers7020815. PMC 4491690. PMID 26010605.
- ↑ Loibl et al. 2021, "Epidemiology and risk factors".
- ↑ "Cancer". World Health Organization. 12 September 2018. Archived from the original on 8 March 2020. Retrieved 16 July 2020.
- ↑ Balasubramanian R, Rolph R, Morgan C, Hamed H (2019). "Genetics of breast cancer: management strategies and risk-reducing surgery". Br J Hosp Med (Lond). 80 (12): 720–725. doi:10.12968/hmed.2019.80.12.720. PMID 31822191. S2CID 209314404.
- 1 2 "World Cancer Report". International Agency for Research on Cancer. 2008. Archived from the original on 31 December 2011. Retrieved 26 February 2011. (cancer statistics often exclude non-melanoma skin cancers such as basal-cell carcinoma, which are common but rarely fatal)
- ↑ "Stewart B. W. and Kleihues P. (Eds): World Cancer Report. IARCPress. Lyon 2003". Archived from the original on 20 October 2008.
- ↑ Wyld L, Markopoulos C, Leidenius M, Senkus-Konefka E, eds. (2018). Breast cancer management for surgeons: a European multidisciplinary textbook. Springer. p. 580. ISBN 978-3-319-56671-9.
- ↑ Laurance J (29 September 2006). "Breast cancer cases rise 80% since Seventies". The Independent. London. Archived from the original on 25 April 2008. Retrieved 9 October 2006.
- ↑ "Breast Cancer: Statistics on Incidence, Survival, and Screening". Imaginis Corporation. 2006. Archived from the original on 24 October 2006. Retrieved 9 October 2006.
- ↑ Breast Cancer: Breast Cancer in Young Women Archived 10 September 2009 at the Wayback Machine WebMD. Retrieved 9 September 2009
- ↑ Nearly 85% of women diagnosed with breast cancer now survive for 5 year or more Archived 5 November 2013 at the Wayback Machine Office for National Statistics, 2013
- ↑ Cancer Stat Facts: Female Breast Cancer Archived 28 May 2019 at the Wayback Machine, U.S. National Cancer Institute, accessed 16 February 2018
- ↑ Coombs NJ, Boyages J (October 2005). "Multifocal and multicentric breast cancer: does each focus matter?". Journal of Clinical Oncology. 23 (30): 7497–7502. doi:10.1200/JCO.2005.02.1147. PMID 16234516.
- ↑ Neri A, Marrelli D, Megha T, Bettarini F, Tacchini D, De Franco L, Roviello F (January 2015). ""Clinical significance of multifocal and multicentric breast cancers and choice of surgical treatment: a retrospective study on a series of 1158 cases"". BMC Surgery. 15 (1): 1. doi:10.1186/1471-2482-15-1. PMC 4324662. PMID 25586679.
- 1 2 3 4 5 Lang Z, Wu Y, Li C, Li X, Wang X, Qu G (August 2017). "Multifocal and Multicentric Breast Carcinoma: A Significantly More Aggressive Tumor than Unifocal Breast Cancer". Anticancer Research. 37 (8): 4593–4598. doi:10.21873/anticanres.11858. PMID 28739757.
- ↑ Narod SA (March 2014). "Bilateral breast cancers". Nature Reviews. Clinical Oncology. 11 (3): 157–166. doi:10.1038/nrclinonc.2014.3. PMID 24492834. S2CID 601112.
- ↑ "Breast-conserving Surgery (Lumpectomy) | Treating Breast Cancer". www.cancer.org. Archived from the original on 2 October 2022. Retrieved 24 March 2022.
- 1 2 Kapoor NS, Chung A, Huynh K, Giuliano AE (December 2012). "Preliminary results: double lumpectomies for multicentric breast carcinoma". The American Surgeon. 78 (12): 1345–1348. doi:10.1177/000313481207801226. PMID 23265123. S2CID 26112023.
- 1 2 Nguyen QD, Tavana A, Sadruddin S, Chao C (August 2020). "Successful Lumpectomy in a Patient With Multicentric Breast Cancer". Cureus. 12 (8): e10072. doi:10.7759/cureus.10072. PMC 7522052. PMID 32999790.
- ↑ "Another Study Looks at Quality of Life After Preventive Mastectomy". www.breastcancer.org. Archived from the original on 2 October 2022. Retrieved 24 March 2022.
- 1 2 3 4 5 6 7 8 9 10 Olson JS (2002). Bathsheba's breast: women, cancer & history. The Johns Hopkins University Press. ISBN 978-0-8018-6936-5.
- 1 2 "Oldest evidence of breast cancer found in Egyptian skeleton". Reuters. 24 March 2015. Archived from the original on 27 March 2015. Retrieved 25 March 2015.
- ↑ "The History of Cancer". American Cancer Society. 25 March 2002. Archived from the original on 9 October 2006. Retrieved 9 October 2006.
- ↑ Yalom M (1997). A history of the breast. New York: Alfred A. Knopf. p. 234. ISBN 978-0-679-43459-7.
- ↑ Faguet G (2015). "Chapter 2: An Historical Overview: From Prehistory to WWII. From Medieval Europe to World War II". The Conquest of Cancer: A Distant Goal. Springer. p. 24. ISBN 9789401791656.
- ↑ Kaartinen M (2013). "Chapter 2: "But Sad Resources": Treating Cancer in the Eighteenth Century". Breast cancer in the eighteenth century. London: Pickering & Chatto. p. 53. ISBN 978-1-84893-364-4.
- 1 2 3 Winchester DJ, Winchester DP, Hudis CA, Norton L (2006). Breast Cancer. PMPH-USA. ISBN 9781550092721.
- 1 2 3 de Moulin D (2013). A short history of breast cancer. Springer Science & Business Media. ISBN 9789401706018.
- ↑ Boddice RG (2014). Pain and Emotion in Modern History. Springer. p. 24. ISBN 9781137372437.
- ↑ Macintyre IM (June 2011). "Scientific surgeon of the Enlightenment or 'plagiarist in everything': a reappraisal of Benjamin Bell (1749–1806)". The Journal of the Royal College of Physicians of Edinburgh. 41 (2): 174–81. doi:10.4997/JRCPE.2011.211. PMID 21677925.

- ↑ Aronowitz RA (2007). Unnatural history: breast cancer and American society. Cambridge, UK: Cambridge University Press. pp. 22–24. ISBN 978-0-521-82249-7.
- ↑ Scientific American, "The Treatment of Cancer by Pressure". Munn & Company. 10 August 1878. p. 86.
- ↑ Morabia A (2004). A History of Epidemiologic Methods and Concepts. Boston: Birkhauser. pp. 301–302. ISBN 978-3-7643-6818-0. Archived from the original on 14 January 2023. Retrieved 31 December 2007.
- 1 2 Knopf-Newman MJ (2004). Beyond Slash, Burn, and Poison: Transforming Breast Cancer Stories Into Action. Rutgers University Press. ISBN 9780813534718.
- ↑ Lacroix M (2011). A Concise History of Breast Cancer. USA: Nova Science Publishers. pp. 59–68. ISBN 978-1-61122-305-7.
- 1 2 3 4 5 6 7 8 9 Sulik GA (2010). Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health. USA: Oxford University Press. ISBN 978-0-19-974045-1. OCLC 535493589.
- ↑ Riter B. "History of Breast Cancer Advocacy". Cancer Resource Center of the Finger Lakes. Archived from the original on 23 June 2013. Retrieved 29 June 2013.
- 1 2 Klawiter M (2008). The Biopolitics of Breast Cancer: Changing Cultures of Disease and Activism. University of Minnesota Press. ISBN 9780816651078.
- ↑ Landeman A (11 June 2008). "Pinkwashing: Can Shopping Cure Breast Cancer?". Center for Media and Democracy. Archived from the original on 5 June 2011.
- ↑ Breast cancer month overshadowed by 'pinkwashing' Archived 12 October 2010 at the Wayback Machine 9 October 2010, Angela Mulholland, CTV.ca News
- ↑ King S (2006). Pink ribbons, inc.: breast cancer and the politics of philanthropy. Minneapolis: University of Minnesota Press. ISBN 0-8166-4898-0.
- ↑ Ehrenreich B (November 2001). "Welcome to Cancerland". Harper's Magazine. Archived from the original on 20 November 2010.
- 1 2 Aschwanden C (17 August 2009). "The Trouble with Mammograms". Los Angeles Times. Archived from the original on 4 December 2010.
- ↑ Olopade OI, Falkson CI (2010). Breast Cancer in Women of African Descent. Springer Science & Business Media. p. 5. ISBN 9781402036644.
- 1 2 3 4 Yedjou CG, Sims JN, Miele L, Noubissi F, Lowe L, Fonseca DD, et al. (3 January 2020). "Health and Racial Disparity in Breast Cancer". Breast Cancer Metastasis and Drug Resistance. Advances in Experimental Medicine and Biology. Vol. 1152. pp. 31–49. doi:10.1007/978-3-030-20301-6_3. ISBN 978-3-030-20300-9. PMC 6941147. PMID 31456178.
- ↑ Baird J, Yogeswaran G, Oni G, Wilson EE (January 2021). "What can be done to encourage women from Black, Asian and minority ethnic backgrounds to attend breast screening? A qualitative synthesis of barriers and facilitators". Public Health. 190: 152–159. doi:10.1016/j.puhe.2020.10.013. PMID 33419526. S2CID 231300410. Archived from the original on 18 April 2023. Retrieved 23 February 2023.
- 1 2 "Reproductive History and Cancer Risk". National Cancer Institute. 30 November 2016. Archived from the original on 4 August 2019. Retrieved 22 August 2019.
- ↑ Azim HA, Santoro L, Russell-Edu W, Pentheroudakis G, Pavlidis N, Peccatori FA (November 2012). "Prognosis of pregnancy-associated breast cancer: a meta-analysis of 30 studies". Cancer Treatment Reviews. 38 (7): 834–42. doi:10.1016/j.ctrv.2012.06.004. PMID 22785217.
- ↑ Schedin P (April 2006). "Pregnancy-associated breast cancer and metastasis". Nature Reviews. Cancer. 6 (4): 281–91. doi:10.1038/nrc1839. PMID 16557280. S2CID 9085879.
- 1 2 3 4 5 6 7 Yarbro CH, Wujcik D, Gobel BH, eds. (2011). Cancer nursing: principles and practice (7th ed.). Jones & Bartlett Publishers. pp. 901–905. ISBN 978-1-4496-1829-2.
- 1 2 Gonçalves V, Sehovic I, Quinn G (2013). "Childbearing attitudes and decisions of young breast cancer survivors: a systematic review". Human Reproduction Update. 20 (2): 279–92. doi:10.1093/humupd/dmt039. PMC 3922144. PMID 24077938.
- ↑ Patel A, Schwarz EB (September 2012). "Cancer and contraception. Release date May 2012. SFP Guideline #20121". Contraception. 86 (3): 191–8. doi:10.1016/j.contraception.2012.05.008. PMID 22682881.
- ↑ McNaught J, Reid RL (July 2006). "Progesterone-only and non-hormonal contraception in the breast cancer survivor: Joint Review and Committee Opinion of the Society of Obstetricians and Gynaecologists of Canada and the Society of Gynecologic Oncologists of Canada". Journal of Obstetrics and Gynaecology Canada. 28 (7): 616–626. doi:10.1016/S1701-2163(16)32195-8. PMID 16924781.
- ↑ Management of the menopause after breast cancer, from the Royal Australian and New Zealand College of Obstetricians and Gynaecologists. College Statement C-Gyn 15. 1st Endorsed: February 2003. Current: November 2011. Review: November 2014
- ↑ Venur VA, Leone JP (September 2016). "Targeted Therapies for Brain Metastases from Breast Cancer". International Journal of Molecular Sciences. 17 (9): 1543. doi:10.3390/ijms17091543. PMC 5037817. PMID 27649142.
- ↑ Suryawanshi YR, Zhang T, Essani K (March 2017). "Oncolytic viruses: emerging options for the treatment of breast cancer". Medical Oncology. 34 (3): 43. doi:10.1007/s12032-017-0899-0. PMID 28185165. S2CID 44562857.
- ↑ Obermiller PS, Tait DL, Holt JT (1999). "Gene therapy for carcinoma of the breast: Therapeutic genetic correction strategies". Breast Cancer Research. 2 (1): 28–31. doi:10.1186/bcr26. PMC 521211. PMID 11250690.
- ↑ Roth JA, Swisher SG, Meyn RE (October 1999). "p53 tumor suppressor gene therapy for cancer". Oncology. 13 (10 Suppl 5): 148–54. PMID 10550840.
- ↑ Yu LY, Tang J, Zhang CM, Zeng WJ, Yan H, Li MP, Chen XP (January 2017). "New Immunotherapy Strategies in Breast Cancer". International Journal of Environmental Research and Public Health. 14 (1): 68. doi:10.3390/ijerph14010068. PMC 5295319. PMID 28085094.
- ↑ San Antonio Breast Cancer Symposium Archived 16 May 2010 at the Wayback Machine Abstracts, newsletters, and other reports of the meeting.
- ↑ Goldhirsch A, Ingle JN, Gelber RD, Coates AS, Thürlimann B, Senn HJ (August 2009). "Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009". Annals of Oncology. 20 (8): 1319–29. doi:10.1093/annonc/mdp322. PMC 2720818. PMID 19535820.
- ↑ "What's new in breast cancer research and treatment?". Cancer. Archived from the original on 12 November 2015. Retrieved 17 November 2015.
- ↑ "Fenretinide (4-HPR): A Preventive Chance for Women at Genetic and Familial Risk?". hindawi. Archived from the original on 17 November 2015. Retrieved 17 November 2015.
- ↑ Burris HA (March 2018). "Ribociclib for the treatment of hormone receptor-positive, human epidermal growth factor receptor 2-negative advanced breast cancer". Expert Review of Anticancer Therapy. 18 (3): 201–213. doi:10.1080/14737140.2018.1435275. PMID 29457921. S2CID 3425945.
- ↑ Gallagher M, Jones DJ, Bell-Syer SV, et al. (Cochrane Wounds Group) (September 2019). "Prophylactic antibiotics to prevent surgical site infection after breast cancer surgery". The Cochrane Database of Systematic Reviews. 2019 (9): CD005360. doi:10.1002/14651858.CD005360.pub5. PMC 6953223. PMID 31557310.
- ↑ Sabel MS (July 2014). "Nonsurgical ablation of breast cancer: future options for small breast tumors". Surgical Oncology Clinics of North America. 23 (3): 593–608. doi:10.1016/j.soc.2014.03.009. PMID 24882353.
- 1 2 Roubidoux MA, Yang W, Stafford RJ (March 2014). "Image-guided ablation in breast cancer treatment". Techniques in Vascular and Interventional Radiology. 17 (1): 49–54. doi:10.1053/j.tvir.2013.12.008. PMID 24636331. S2CID 24372526.
- ↑ Fornage BD, Hwang RF (August 2014). "Current status of imaging-guided percutaneous ablation of breast cancer". AJR. American Journal of Roentgenology. 203 (2): 442–8. doi:10.2214/AJR.13.11600. PMID 25055283.
- ↑ Duffy MJ (July 2001). "Biochemical markers in breast cancer: which ones are clinically useful?". Clinical Biochemistry. 34 (5): 347–52. doi:10.1016/s0009-9120(00)00201-0. PMID 11522269.
Works cited
- Harbeck N, Penault-Llorca F, Cortes J, Gnant M, Houssami N, Poortmans P, Ruddy K, Tsang J, Cardoso F (September 2019). "Breast cancer". Nat Rev Dis Primers. 5 (1): 66. doi:10.1038/s41572-019-0111-2. PMID 31548545. S2CID 202718231.
- Hayes DF, Lippman ME (2022). "79: Breast Cancer". In Loscalzo J, Fauci A, Kasper D, et al. (eds.). Harrison's Principles of Internal Medicine (21 ed.). McGraw Hill. ISBN 978-1-264-26850-4.
- Loibl S, Poortmans P, Morrow M, Denkert C, Curigliano G (May 2021). "Breast cancer". Lancet. 397 (10286): 1750–1769. doi:10.1016/S0140-6736(20)32381-3. PMID 33812473. S2CID 232485291.
- Menes TS, Coster D, Coster D, Shenhar-Tsarfaty S (October 2021). "Contribution of clinical breast exam to cancer detection in women participating in a modern screening program". BMC Womens Health. 21 (1): 368. doi:10.1186/s12905-021-01507-x. PMC 8524962. PMID 34666735.
- Metaxa L, Healy NA, O'Keeffe SA (November 2019). "Breast microcalcifications: the UK RCR 5-point breast imaging system or BI-RADS; which is the better predictor of malignancy?". Br J Radiol. 92 (1103): 20190177. doi:10.1259/bjr.20190177. PMC 6849664. PMID 31365279.
- Nielsen S, Narayan AK (February 2023). "Breast Cancer Screening Modalities, Recommendations, and Novel Imaging Techniques". Surg Clin North Am. 103 (1): 63–82. doi:10.1016/j.suc.2022.08.004. PMID 36410354. S2CID 252990902.
- Rahman WT, Helvie MA (September 2022). "Breast cancer screening in average and high-risk women". Best Pract Res Clin Obstet Gynaecol. 83: 3–14. doi:10.1016/j.bpobgyn.2021.11.007. PMID 34903436. S2CID 244447464.
External links
| Library resources about Breast cancer |