Asthma triggers are factors or stimuli that provoke the exacerbation of asthma symptoms or increase the degree of airflow disruption, which can lead to an asthma attack.[1] An asthma attack is characterized by an obstruction of the airway, hypersecretion of mucus and bronchoconstriction due to the contraction of smooth muscles around the respiratory tract. Its symptoms include a wide range of manifestations such as breathlessness, coughing, a tight chest and wheezing.[2]
An asthma attack is usually mediated by an inflammatory pathway, where a trigger such as an allergen could lead to a series of immune response mediated by various types of immune cells.[3]
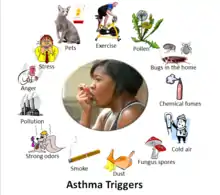
Common triggers for asthma include allergens like pet dander, dust mites, pollens and molds. Other types of triggers like exercise, air pollutants, tobacco smoke, humidity, cold air, or certain medicines may also play a role in triggering asthma.[4] While it has been proposed that asthma triggers can be classified into three types: allergic triggers, environmental triggers and physical triggers, a universal categorization of asthma triggers has yet to be done.[4] Other studies have also classified asthma triggers into psychological factors, air pollutants, physical activity, allergens and infection.[5]
Asthma is an extremely common chronic disease affecting over 26 million people and 7 million children in the US.[3] Recognizing the trigger for asthma and avoiding it can be a simple yet effective way to deal with the disease and avoid an asthma attack.[6] Although a cure for asthma is yet to be invented, various treatment methods are available for both long-term control and immediate relieve of an asthma attack.[7]
Pathophysiology

The pathophysiology for asthma mainly involves the inflammatory pathway, associated with several types of immune cells in the body, mainly T helper 2 cells (Th2 cells), B cells and mast cells. In a nut shell, as a stimulus, such as an allergen comes into contact with an asthma patient, it activates various types of immune cells leading to an inflammatory response, causing bronchial hyperresponsiveness, bronchoconstriction, excessive mucus secretion, airflow obstruction and an asthma attack.[3] A more detail rundown of the process is provided below.
First, during the sensitization phase, where T cells interact with dendritic cells, the dendritic cells will present a specific antigen from the allergen to Th2 cells, leading to their development.[8] Afterward, the activated Th2 cells would release interleukine-4, a type of cytokine to promote B cells, another type of immune cell to differentiate intoallergen-specific memory B cells and plasma cells.[9] The plasma cells will then extensively produce allergen-specific IgE antibodies, which are captured by a type of receptor, FceRI, on the mast cells.[9]
Mast cells are immune cells usually located at tissues exposed to the environment, such as the skin, respiratory tract mucosa and digestive tract mucosa.[10] They are equipped with preformed granules loaded with vasoactive amines and proteases.[11] As the FceRI receptors on mast cells capture the IgE antibodies produced by Th2 cells, they become sensitive to the specific allergen.

Due to this, the mast cells will be activated when they are exposed to the specific allergen. As an allergen binds to the IgE antibodies on the mast cell surface, clustering and cross-link formation of FceRI takes place.[12][10] This leads to the recruitment and activation of several tyrosine kinases, a type of enzyme that phosphorylates protein.[13] Consequently, these kinase activation contributes to intracellular Ca2+ influx after a series of reaction. The Ca2+ level surge results in cytoskeletal rearrangement, allowing exocytosis and degranulation of intracellular granules, thus releasing vasoactive amines and proteases.[14] These vasoactive amines such as histamine, heparin and serotonin released from the mast cell granules cause vasodilation, increased vascular permeability, smooth muscle contraction and increased mucus secretion. Mast cells degranulation also results in the release of eosinophil chemotactic factors and neutrophil chemotactic factors. These factors attract eosinophils and neutrophils from the body respectively, which can intensify the inflammation response.[15] Moreover, the elevated Ca2+ level also leads to arachidonic acid enzymatic pathway activation, contributing to the release of lipid mediators.[16] These lipid mediators, particularly prostaglandins and leukotrienes elicit vasodilation, increased vascular permeability and smooth muscle contraction.[17] Moreover, the increase in Ca2+ level also leads to activation of certain transcription factors which induces pro-inflammatory cytokines transcription.[18] These pro-inflammatory cytokines such as TNF, Interleukin-1 and Interleukin-8 lead to acute inflammation and leukocyte recruitment.[19]
Examples of asthma triggers

Allergic triggers
Allergic triggers are factors or chemicals that could induce airway sensitization, inflammation, bronchospasm and other asthmatic symptoms.[20]
Allergens are the most common trigger for allergic asthma. Examples of such triggers of asthma include naturally occurring aeroallergens like house dust mites, animal feces and pollen.[21] Pets, molds and pests are also potential triggers.[22] When an asthma patient inhales or come into contact withsuch allergen, mast cells in the airway tract releases vasoactive amines and proteases. This leads to a release of cytokines and mediates a broad range of inflammatory and allergic responses.[19]
Environmental triggers
In addition to allergens, studies have revealed that environmental factors may also increase the risk of triggering an asthma attack.[21][23] Examples of these factors include respiratory tract viral infections,[24] exposure to air pollutants such as ozone[25] or a change in lifestyle that involves a decrease in exposure to microbes and their products like endotoxin.[26] Although its mechanism of action is still unknown, an in vivo study[21] has demonstrated that these environmental factors lead to the accumulation of neutrophil extracellular traps (NET) releasing neutrophils in the lungs. This increased release of NETs have been found to be associated with asthmatic symptoms such as mucus hypersecretion.[27]
Another environmental risk factor is exposure to formaldehyde.[28] Formaldehyde itself is a chemical that can cause irritation to the respiratory tract. In addition, it may react with macromolecules such as albumin which can induce the production of igE antibodies which can bind to mast cells and lead to hyperresponsiveness of the respiratory tract.[28]
Exercise
Exercise induced asthma is common in most asthma patients.[29] Although the mechanism for such a phenomenon is still unclear, researchers have proposed that as the body gasps for more oxygen during exercise, more cold and dry air is inhaled. The passage of this cold and dry air causes a loss of moisture from the mucosal membrane of the respiratory tract. The osmolarity changes brought by such action can lead to an increased release of proinflammatory mediators such as cytokines, leading to a hypersensitivity of the airway.[30][31] Cooling of the respiratory tract may also activate cholinergic receptors, which can induce bronchoconstriction and mucus secretion, further narrowing the airway.[32] Swimmers with asthma may also inhale an excess amount of contaminated and irritating air with compound derived from chlorine gas, this can increase the risk of an asthma attack.[33]
Medications
Aspirin induced asthma, or aspirin-exacerbated respiratory disease, refers to situations where the use of aspirin worsen the asthma conditions.[34] Other non-steroidal anti-inflammatory drugs (NSAIDs) that inhibits the enzyme, cyclooxygenase-1, may also lead to an asthma attack.
After the inhibition of cyclooxygenase-1 enzyme by the NSAIDs, an accumulation of arachidonic acid will be resulted. This, in turn, would increase the production of leukotrienes. Leukotrienes is an inflammatory mediator. The accumulation of proinflammatory leukotrienes would overstimulate the cysteinyl leukotriene receptors in the respiratory system, leading to bronchoconstriction and the over-secretion of mucus, thus blocking the airway.[34]
Beta-blocker, or beta-adrenergic antagonists, may also induce bronchial constriction and block the action of other beta-receptor targeted asthmatic drugs, leading to a worsening asthma condition.[35] Therefore, asthma patients should be cautious and inform their physicians of their asthma conditions.[36]
Occupational asthma triggers
Occupational asthma refers to a type of asthma that is resulted from repeated exposure to an agent that causes or exacerbates asthma in a workplace.[37] Although the primary cause for occupational asthma varies from situation to situation, common agents such as metal, diesel, cleaning agents, dimethylsulphate, diisocyanates, latex, persulfate, aldehydes, isocyanates, wood dusts and flour should be handled with great care.[38][39][40]
Tobacco smoke
Both first-hand and second-hand tobacco smoke can be a trigger for asthma attack.[41] It may worsen the condition of asthma as it is an irritant and induces bronchoconstriction.[42]
Psychological triggers
Studies have also indicated that psychological stress may be associated with a higher chance of asthma attack.[5] Patients with psychological stress are found to have a reduced awareness of controlling asthma and a less desirable physical health.[5][43]
Symptom
One of the clinical asthmatic symptoms is shortness of breath due to narrowing of the respiratory tract, caused by mucus plug formation and bronchoconstriction as smooth muscles contract.[44] Another typical symptom is wheezing. During expiration, turbulent airflow crushes the narrowed respiratory tract, leading to a wheezing sound.[45] Moreover, the increased mucus secretion may not be limited to the respiratory tract, and other symptoms such as watery eyes and rhinitis are also common.[45] Furthermore, increased vasodilation and vascular permeability may result in angioedema, the swelling of the skin, and hives.[46] In severe complications, as ventilation is impaired, acute respiratory failure may occur due to the inadequate amount of oxygen in the circulatory system.[47] Another life-threatening condition is pneumothorax, the collapse of the lungs due to hyperinflation.[48]
Avoidance
Understanding the specific asthma triggers for a patient and avoiding them can be a simple way for preventing an asthma attack.[41] Regularly washing beddings, quitting smoking, doing pest controls, keeping a sensitized living environment, removing stagnant water, avoiding products with potential irritants, etc., can be effective in avoiding an asthma attack.[41]
Education about asthma triggers should be done by physicians to help patients understand what activities or materials should be avoided. Reduction of exposure to asthma triggers should be done by asthmatic patient as well.[4] Parents of asthmatic children should also be cautious of common asthma triggers in order to reduce risks of an asthma attack.[22]
Treatment

Quick-relief medicine
Quick-relief medicine are used for treating an acute asthma attack. The first line of medicine for treating this situation is short-term beta-2-adrenoreceptor agonists, which are drugs that can stimulate the beta-2 adrenergic receptors. They are bronchodilators and can effectively relieve the symptoms by clearing the airway. Examples include albuterol and levalbuterol.[7] Commonly they are used with a portable inhaler which allows the patient to administer the medicine at once during an attack.
Another common medicine for an acute attack is anticholinergic drugs such as ipratropium and tiotropium, which are also bronchodilators.[7] They work by blocking off the cholinergic receptors and reduces mucus secretion and bronchoconstriction.[7]
Another type of treatment for acute asthma attack is immunosuppressive drugs like corticosteroids, which can also alleviate an asthmatic response.[49] Examples include prednisone and methyl prednisone which are usually administered orally or intravenously for treating an acute situation.[7] However, note that long term use of corticosteroids may lead to severe side effects.
Long-term control
Continuous and long-term use of certain medicines can help reduce the risk of an asthma attack and keep the disease under control.

Long term use of certain types of corticosteroids, such as fluticasone propionate may be administered through the pulmonary route to reduce the risk of an asthma attack.[50]
Oral use of leukotriene receptor antagonist such as Zafirlukast may also be used as a long term control for asthma in addition to corticosteroids.[51][52]
Moreover, another option is the use of cromolyn sodium, which can prevent an asthma attack by halting Ca2+ influx, thus preventing mast cell degranulation and subsequent asthmatic complications [53]
Other than drugs, an alternative treatment method is de-sensitization, which involves exposure to a well-controlled, small and increasing amounts of specific allergen over a long duration of time.[54] The rationale is to trigger antigen competition by the development of allergen-specific IgG antibodies, which can reduce to risk of an allergic response.[54]
Long-acting beta-agonists such as salmetrol had been used in combination with corticosteroids to control asthma symptoms. They are drugs that can stimulate the beta-2 adrenergic receptors and mediate a bronchodilation effect for over 12 hours. However, a recent study in 2010 has found that this treatment method could increase the risk of asthma-related deaths and intubations.[55] The Food and Drug Administration (FDA) is also recommending the discontinuation of the drug if asthma control has been achieved.[56]
References
- ↑ "Trigger", McGraw-Hill Concise Dictionary of Modern Medicine, retrieved 2022-03-29
- ↑ British Thoracic Society; Scottish Intercollegiate Guidelines Network (2014). "British guideline on the management of asthma". Thorax. 69 (Suppl 1): 1–192. ISSN 1468-3296. PMID 25323740.
- 1 2 3 Morris. M, MD, FACP, FCCP (2021-05-03). "Asthma: Practice Essentials, Background, Anatomy". Medscape.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 Vernon, Margaret K.; Wiklund, Ingela; Bell, Jill A.; Dale, Peter; Chapman, Kenneth R. (2012-11-19). "What Do We Know about Asthma Triggers? A Review of the Literature". Journal of Asthma. 49 (10): 991–998. doi:10.3109/02770903.2012.738268. ISSN 0277-0903. PMID 23574397. S2CID 38294258.
- 1 2 3 Ritz, Thomas; Steptoe, Andrew; Bobb, Carol; Harris, Alexander H. S.; Edwards, Martin (2006). "The Asthma Trigger Inventory: Validation of a Questionnaire for Perceived Triggers of Asthma". Psychosomatic Medicine. 68 (6): 956–965. doi:10.1097/01.psy.0000248898.59557.74. ISSN 0033-3174. PMID 17132841. S2CID 31788889.
- ↑ Viswam, Darsana; Mansur, Adel H. (2020). "Mode of onset and triggers of severe asthma". Annals of Allergy, Asthma & Immunology. 128 (4): 466–467. doi:10.1016/j.anai.2022.01.006. ISSN 1081-1206. PMID 35031415. S2CID 245916683.
- 1 2 3 4 5 Bissell, Karen; Ellwood, Philippa; Ellwood, Eamon; Chiang, Chen-Yuan; Marks, Guy; El Sony, Asma; Asher, Innes; Billo, Nils; Perrin, Christophe (2019-02-19). "Essential Medicines at the National Level: The Global Asthma Network's Essential Asthma Medicines Survey 2014". International Journal of Environmental Research and Public Health. 16 (4): 605. doi:10.3390/ijerph16040605. ISSN 1660-4601. PMC 6406388. PMID 30791442.
- ↑ Humeniuk, Piotr; Dubiela, Pawel; Hoffmann-Sommergruber, Karin (2017-07-11). "Dendritic Cells and Their Role in Allergy: Uptake, Proteolytic Processing and Presentation of Allergens". International Journal of Molecular Sciences. 18 (7): 1491. doi:10.3390/ijms18071491. ISSN 1422-0067. PMC 5535981. PMID 28696399.
- 1 2 Saunders, Sean P.; Ma, Erica G. M.; Aranda, Carlos J.; Curotto de Lafaille, Maria A. (2019-04-26). "Non-classical B Cell Memory of Allergic IgE Responses". Frontiers in Immunology. 10: 715. doi:10.3389/fimmu.2019.00715. ISSN 1664-3224. PMC 6498404. PMID 31105687.
- 1 2 Holgate, Stephen T (2013). "Mechanisms of Asthma and Implications for Its Prevention and Treatment: A Personal Journey". Allergy, Asthma & Immunology Research. 5 (6): 343–347. doi:10.4168/aair.2013.5.6.343. ISSN 2092-7355. PMC 3810539. PMID 24179679.
- ↑ Bradding, P; Feather, I H; Howarth, P H; Mueller, R; Roberts, J A; Britten, K; Bews, J P; Hunt, T C; Okayama, Y; Heusser, C H (1992-11-01). "Interleukin 4 is localized to and released by human mast cells". Journal of Experimental Medicine. 176 (5): 1381–1386. doi:10.1084/jem.176.5.1381. ISSN 0022-1007. PMC 2119427. PMID 1402683. S2CID 7033172.
- ↑ Beasley, Richard; Roche, William R.; Roberts, J. Alan; Holgate, Stephen T. (1989). "Cellular Events in the Bronchi in Mild Asthma and after Bronchial Provocation". American Review of Respiratory Disease. 139 (3): 806–817. doi:10.1164/ajrccm/139.3.806. ISSN 0003-0805. PMID 2923380.
- ↑ Gilfillan, Alasdair M.; Rivera, Juan (2009). "The tyrosine kinase network regulating mast cell activation". Immunological Reviews. 228 (1): 149–169. doi:10.1111/j.1600-065x.2008.00742.x. ISSN 0105-2896. PMC 2669301. PMID 19290926.
- ↑ Klein, Ofir; Sagi-Eisenberg, Ronit (2019-03-18). "Anaphylactic Degranulation of Mast Cells: Focus on Compound Exocytosis". Journal of Immunology Research. 2019: 1–12. doi:10.1155/2019/9542656. ISSN 2314-8861. PMC 6442490. PMID 31011586.
- ↑ Goetzl, E J; Austen, K F (1976-12-01). "Structural determinants of the eosinophil: chemotactic activity of the acidic tetrapeptides of eosinophil chemotactic factor of anaphylaxis". Journal of Experimental Medicine. 144 (6): 1424–1437. doi:10.1084/jem.144.6.1424. ISSN 0022-1007. PMC 2190483. PMID 1003098.
- ↑ Ong, W.-Y.; Farooqui, T.; Farooqui, A.A. (2010-09-01). "Involvement of Cytosolic Phospholipase A2, Calcium Independent Phospholipase A2 and Plasmalogen Selective Phospholipase A2 in Neurodegenerative and Neuropsychiatric Conditions". Current Medicinal Chemistry. 17 (25): 2746–2763. doi:10.2174/092986710791859289. ISSN 0929-8673. PMID 20586719.
- ↑ Funk, Colin D. (2001-11-30). "Prostaglandins and Leukotrienes: Advances in Eicosanoid Biology". Science. 294 (5548): 1871–1875. Bibcode:2001Sci...294.1871F. doi:10.1126/science.294.5548.1871. ISSN 0036-8075. PMID 11729303.
- ↑ Cargnello, Marie; Roux, Philippe P. (2011). "Activation and Function of the MAPKs and Their Substrates, the MAPK-Activated Protein Kinases". Microbiology and Molecular Biology Reviews. 75 (1): 50–83. doi:10.1128/mmbr.00031-10. ISSN 1092-2172. PMC 3063353. PMID 21372320.
- 1 2 Zhang, Jun-Ming; An, Jianxiong (2007). "Cytokines, Inflammation, and Pain". International Anesthesiology Clinics. 45 (2): 27–37. doi:10.1097/aia.0b013e318034194e. ISSN 0020-5907. PMC 2785020. PMID 17426506.
- ↑ D'Amato, M; Cecchi, L; Annesi-Maesano, I; D'Amato, G (2018-04-16). "News on Climate Change, Air Pollution, and Allergic Triggers of Asthma". Journal of Investigational Allergology and Clinical Immunology. 28 (2): 91–97. doi:10.18176/jiaci.0228. ISSN 1018-9068. PMID 29345235.
- 1 2 3 Radermecker, Coraline; Sabatel, Catherine; Vanwinge, Céline; Ruscitti, Cecilia; Maréchal, Pauline; Perin, Fabienne; Schyns, Joey; Rocks, Natacha; Toussaint, Marie; Cataldo, Didier; Johnston, Sebastian L (2019). "Locally instructed CXCR4hi neutrophils trigger environment-driven allergic asthma through the release of neutrophil extracellular traps". Nature Immunology. 20 (11): 1444–1455. doi:10.1038/s41590-019-0496-9. ISSN 1529-2908. PMC 6859073. PMID 31591573.
- 1 2 Morgan, Wayne J.; Crain, Ellen F.; Gruchalla, Rebecca S.; O'Connor, George T.; Kattan, Meyer; Evans, Richard; Stout, James; Malindzak, George; Smartt, Ernestine; Plaut, Marshall; Walter, Michelle (2004-09-09). "Results of a Home-Based Environmental Intervention among Urban Children with Asthma". New England Journal of Medicine. 351 (11): 1068–1080. doi:10.1056/nejmoa032097. ISSN 0028-4793. PMID 15356304.
- ↑ Eder, Waltraud; Ege, Markus J.; von Mutius, Erika (2006-11-23). "The Asthma Epidemic". New England Journal of Medicine. 355 (21): 2226–2235. doi:10.1056/NEJMra054308. ISSN 0028-4793. PMID 17124020.
- ↑ Busse, William W; Lemanske, Robert F; Gern, James E (2010). "Role of viral respiratory infections in asthma and asthma exacerbations". The Lancet. 376 (9743): 826–834. doi:10.1016/S0140-6736(10)61380-3. PMC 2972660. PMID 20816549.
- ↑ Peden, David B. (2005). "The epidemiology and genetics of asthma risk associated with air pollution". Journal of Allergy and Clinical Immunology. 115 (2): 213–219. doi:10.1016/j.jaci.2004.12.003. ISSN 0091-6749. PMID 15696070.
- ↑ Braun-Fahrländer, Charlotte; Riedler, Josef; Herz, Udo; Eder, Waltraud; Waser, Marco; Grize, Leticia; Maisch, Soyoun; Carr, David; Gerlach, Florian; Bufe, Albrecht; Lauener, Roger P. (2002-09-19). "Environmental Exposure to Endotoxin and Its Relation to Asthma in School-Age Children". New England Journal of Medicine. 347 (12): 869–877. doi:10.1056/nejmoa020057. ISSN 0028-4793. PMID 12239255.
- ↑ Liu, Ting; Wang, Fa-Ping; Wang, Geng; Mao, Hui (2017). "Role of Neutrophil Extracellular Traps in Asthma and Chronic Obstructive Pulmonary Disease". Chinese Medical Journal. 130 (6): 730–736. doi:10.4103/0366-6999.201608. ISSN 0366-6999. PMC 5358425. PMID 28303858.
- 1 2 McGwin, Gerald; Lienert, Jeffrey; Kennedy, John I. (2010). "Formaldehyde Exposure and Asthma in Children: A Systematic Review". Environmental Health Perspectives. 118 (3): 313–317. doi:10.1289/ehp.0901143. ISSN 0091-6765. PMC 2854756. PMID 20064771.
- ↑ Crapo, R. O.; Casaburi, R.; Coates, A. L.; Enright, P. L.; Hankinson, J. L.; Irvin, C. G.; MacIntyre, N. R.; McKay, R. T.; Wanger, J. S.; Anderson, S. D.; Cockcroft, D. W.; Fish, J. E.; Sterk, P. J. (2000). "Guidelines for Methacholine and Exercise Challenge Testing—1999". American Journal of Respiratory and Critical Care Medicine. 161 (1): 309–329. doi:10.1164/ajrccm.161.1.ats11-99. ISSN 1073-449X. PMID 10619836.
- ↑ Raddeley, R (1988). "Surgical management of morbid obesity. W. O. Griffin Jr. 150 × 230 mm. Pp. 284. Illustrated. 1987. New York: Marcel Dekker Inc. $95.50". British Journal of Surgery. 75 (5): 503. doi:10.1002/bjs.1800750554. ISSN 0007-1323.
- ↑ Anderson, Sandra D.; Daviskas, Evangelia (2000). "The mechanism of exercise-induced asthma is …". Journal of Allergy and Clinical Immunology. 106 (3): 453–459. doi:10.1067/mai.2000.109822. ISSN 0091-6749. PMID 10984363.
- ↑ McFADDEN, E. R.; NELSON, JO ANN; SKOWRONSKI, M. E.; LENNER, K. A. (1999). "Thermally Induced Asthma and Airway Drying". American Journal of Respiratory and Critical Care Medicine. 160 (1): 221–226. doi:10.1164/ajrccm.160.1.9810055. ISSN 1073-449X. PMID 10390404.
- ↑ Thickett, K.M.; McCoach, J.S.; Gerber, J.M.; Sadhra, S.; Burge, P.S. (2002-05-01). "Occupational asthma caused by chloramines in indoor swimming-pool air". European Respiratory Journal. 19 (5): 827–832. doi:10.1183/09031936.02.00232802. ISSN 0903-1936. PMID 12030720. S2CID 5788935.
- 1 2 Szczeklik, Andrew; Stevenson, Donald D. (2003). "Aspirin-induced asthma: Advances in pathogenesis, diagnosis, and management". Journal of Allergy and Clinical Immunology. 111 (5): 913–921. doi:10.1067/mai.2003.1487. PMID 12743549.
- ↑ Morales, Daniel R.; Lipworth, Brian J.; Donnan, Peter T.; Jackson, Cathy; Guthrie, Bruce (2017). "Respiratory effect of beta-blockers in people with asthma and cardiovascular disease: population-based nested case control study". BMC Medicine. 15 (1): 18. doi:10.1186/s12916-017-0781-0. ISSN 1741-7015. PMC 5270217. PMID 28126029.
- ↑ "Medicines Can Trigger Asthma". Asthma and allergy foundation of america. 2018. Retrieved 2022-03-29.
- ↑ Tarlo, Susan M.; Lemiere, Catherine (2014-02-13). "Occupational Asthma". New England Journal of Medicine. 370 (7): 640–649. doi:10.1056/nejmra1301758. ISSN 0028-4793. PMID 24521110.
- ↑ "Handling fish can cause occupational asthma". Food and Chemical Toxicology. 35 (9): 930. 1997. doi:10.1016/s0278-6915(97)90051-x. ISSN 0278-6915.
- ↑ Baur, Xaver; Bakehe, Prudence (2014). "Allergens causing occupational asthma: an evidence-based evaluation of the literature". International Archives of Occupational and Environmental Health. 87 (4): 339–363. doi:10.1007/s00420-013-0866-9. ISSN 0340-0131. PMID 23595938. S2CID 38640302.
- ↑ Labrecque, Manon (2012). "Irritant-induced asthma". Current Opinion in Allergy & Clinical Immunology. 12 (2): 140–144. doi:10.1097/aci.0b013e32835143b8. ISSN 1528-4050. PMID 22327170. S2CID 28763190.
- 1 2 3 "Asthma and Secondhand Smoke". Centers for Disease Control and Prevention. 2022-02-11. Retrieved 2022-03-29.
- ↑ Pietinalho, A.; Pelkonen, A.; Rytilä, P. (2009-10-12). "Linkage between smoking and asthma". Allergy. 64 (12): 1722–1727. doi:10.1111/j.1398-9995.2009.02208.x. ISSN 0105-4538. PMID 19832738. S2CID 40233991.
- ↑ Van Lieshout, Ryan J; MacQueen, Glenda (2008). "Psychological Factors in Asthma". Allergy, Asthma & Clinical Immunology. 4 (1): 12–28. doi:10.1186/1710-1492-4-1-12. ISSN 1710-1492. PMC 2869336. PMID 20525122.
- ↑ Frontiers Production, Office (2022-03-23). "Erratum: Mechanisms of Particles in Sensitization, Effector Function and Therapy of Allergic Disease". Frontiers in Immunology. 13: 891445. doi:10.3389/fimmu.2022.891445. ISSN 1664-3224. PMC 8985158. PMID 35401505.
- 1 2 Parker, R. (2007-08-01). "Gibson P. Evidence-based respiratory medicine. Oxford: Blackwell BMJ, 2005". Evidence-Based Medicine. 12 (4): 125. doi:10.1136/ebm.12.4.125. ISSN 1356-5524. S2CID 71255770.
- ↑ Bernstein, Jonathan A; Moellman, Joseph (2012-11-06). "Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema". International Journal of Emergency Medicine. 5 (1): 39. doi:10.1186/1865-1380-5-39. ISSN 1865-1380. PMC 3518251. PMID 23131076. S2CID 9039857.
- ↑ Smyth, Melinda (2005). "Acute Respiratory Failure: Part 2. Failure of Ventilation". American Journal of Nursing. 105 (6): 72AA–72DD. doi:10.1097/00000446-200506000-00040. ISSN 0002-936X.
- ↑ E, Yiannakopoulou (2018-12-21). "Pneumothorax, pneumomediastinum, subcutaneous emphysema: serious complications of asthma". Archives of Asthma, Allergy and Immunology. 2 (1): 016–017. doi:10.29328/journal.aaai.1001014. ISSN 2639-3182. S2CID 80725017.
- ↑ Djukanović, Ratko; Wilson, John W.; Britten, Karen M.; Wilson, Susan J.; Walls, Andrew F.; Roche, William R.; Howarth, Peter H.; Holgate, Stephen T. (1992). "Effect of an Inhaled Corticosteroid on Airway Inflammation and Symptoms in Asthma". American Review of Respiratory Disease. 145 (3): 669–674. doi:10.1164/ajrccm/145.3.669. ISSN 0003-0805. PMID 1546849.
- ↑ Harrison, TW; Oborne, J; Newton, S; Tattersfield, AE (2004). "Doubling the dose of inhaled corticosteroid to prevent asthma exacerbations: randomised controlled trial". The Lancet. 363 (9405): 271–275. doi:10.1016/s0140-6736(03)15384-6. ISSN 0140-6736. PMID 14751699. S2CID 28581643.
- ↑ Choi, Jaehwa; Azmat, Chaudhary Ehtsham (2023), "Leukotriene Receptor Antagonists", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32119332, retrieved 2023-06-20
- ↑ "thuốc trị hen suyễn". Retrieved 20 June 2023.
- ↑ Georgopoulos, Dimitris; Giulekas, Dimitris; Ilonidis, George; Sichletidis, Lazaws (1989). "Effect of Salbutamol, Ipratropium Bromide and Cromolyn Sodium on Prostaglandin F2α -Induced Bronchospasm". Chest. 96 (4): 809–814. doi:10.1378/chest.96.4.809. ISSN 0012-3692. PMID 2529105.
- 1 2 Krishna, M T; Huissoon, A P (2010-12-22). "Clinical immunology review series: an approach to desensitization". Clinical and Experimental Immunology. 163 (2): 131–146. doi:10.1111/j.1365-2249.2010.04296.x. ISSN 0009-9104. PMC 3043304. PMID 21175592.
- ↑ Salpeter, Shelley R.; Wall, Andrew J.; Buckley, Nicholas S. (2010). "Long-acting Beta-Agonists with and without Inhaled Corticosteroids and Catastrophic Asthma Events". The American Journal of Medicine. 123 (4): 322–328.e2. doi:10.1016/j.amjmed.2009.07.035. PMID 20176343.
- ↑ Chowdhury, Badrul A.; Dal Pan, Gerald (2010). "The FDA and Safe Use of Long-Acting Beta-Agonists in the Treatment of Asthma". New England Journal of Medicine. 362 (13): 1169–1171. doi:10.1056/NEJMp1002074. ISSN 0028-4793. PMID 20181964.