Effective dose is a dose quantity in the International Commission on Radiological Protection (ICRP) system of radiological protection.[1]
It is the tissue-weighted sum of the equivalent doses in all specified tissues and organs of the human body and represents the stochastic health risk to the whole body, which is the probability of cancer induction and genetic effects, of low levels of ionizing radiation.[2][3] It takes into account the type of radiation and the nature of each organ or tissue being irradiated, and enables summation of organ doses due to varying levels and types of radiation, both internal and external, to produce an overall calculated effective dose.
The SI unit for effective dose is the sievert (Sv) which represents a 5.5% chance of developing cancer.[4] The effective dose is not intended as a measure of deterministic health effects, which is the severity of acute tissue damage that is certain to happen, that is measured by the quantity absorbed dose.[5]
The concept of effective dose was developed by Wolfgang Jacobi and published in 1975, and was so convincing that the ICRP incorporated it into their 1977 general recommendations (publication 26) as "effective dose equivalent".[6] The name "effective dose" replaced the name "effective dose equivalent" in 1991.[7] Since 1977 it has been the central quantity for dose limitation in the ICRP international system of radiological protection.[1]
Uses

According to the ICRP, the main uses of effective dose are the prospective dose assessment for planning and optimisation in radiological protection, and demonstration of compliance with dose limits for regulatory purposes. The effective dose is thus a central dose quantity for regulatory purposes.[8]
The ICRP also says that effective dose has made a significant contribution to radiological protection as it has enabled doses to be summed from whole and partial body exposure from external radiation of various types and from intakes of radionuclides.[9]
Usage for external dose
The calculation of effective dose is required for partial or non-uniform irradiation of the human body because equivalent dose does not consider the tissue irradiated, but only the radiation type. Various body tissues react to ionising radiation in different ways, so the ICRP has assigned sensitivity factors to specified tissues and organs so that the effect of partial irradiation can be calculated if the irradiated regions are known.[10] A radiation field irradiating only a portion of the body will carry lower risk than if the same field irradiated the whole body. To take this into account, the effective doses to the component parts of the body which have been irradiated are calculated and summed. This becomes the effective dose for the whole body, dose quantity E. It is a "protection" dose quantity which can be calculated, but cannot be measured in practice.
An effective dose will carry the same effective risk to the whole body regardless of where it was applied, and it will carry the same effective risk as the same amount of equivalent dose applied uniformly to the whole body.
Usage for internal dose
Effective dose can be calculated for committed dose which is the internal dose resulting from inhaling, ingesting, or injecting radioactive materials.
The dose quantity used is:
Committed effective dose, E(t) is the sum of the products of the committed organ or tissue equivalent doses and the appropriate tissue weighting factors WT, where t is the integration time in years following the intake. The commitment period is taken to be 50 years for adults, and to age 70 years for children.[11]
Calculation of effective dose
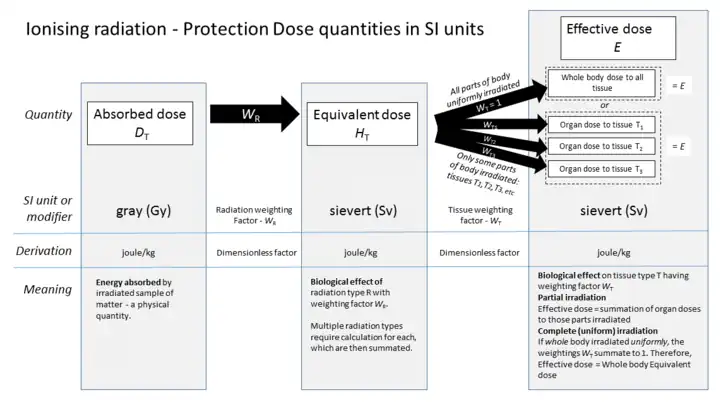
Ionizing radiation deposits energy in the matter being irradiated. The quantity used to express this is the absorbed dose, a physical dose quantity that is dependent on the level of incident radiation and the absorption properties of the irradiated object. Absorbed dose is a physical quantity, and is not a satisfactory indicator of biological effect, so to allow consideration of the stochastic radiological risk, the dose quantities equivalent dose and effective dose were devised by the International Commission on Radiation Units and Measurements (ICRU) and the ICRP to calculate the biological effect of an absorbed dose.
To obtain an effective dose, the calculated absorbed organ dose DT is first corrected for the radiation type using factor WR to give a weighted average of the equivalent dose quantity HT received in irradiated body tissues, and the result is further corrected for the tissues or organs being irradiated using factor WT, to produce the effective dose quantity E.
The sum of effective doses to all organs and tissues of the body represents the effective dose for the whole body. If only part of the body is irradiated, then only those regions are used to calculate the effective dose. The tissue weighting factors summate to 1.0, so that if an entire body is radiated with uniformly penetrating external radiation, the effective dose for the entire body is equal to the equivalent dose for the entire body.
Use of tissue weighting factor WT
The ICRP tissue weighting factors are given in the accompanying table, and the equations used to calculate from either absorbed dose or equivalent dose are also given.
Some tissues like bone marrow are particularly sensitive to radiation, so they are given a weighting factor that is disproportionately large relative to the fraction of body mass they represent. Other tissues like the hard bone surface are particularly insensitive to radiation and are assigned a disproportionally low weighting factor.
| Organs | Tissue weighting factors | ||
|---|---|---|---|
| ICRP26 1977 | ICRP60 1990[13] | ICRP103 2007[14] | |
| Gonads | 0.25 | 0.20 | 0.08 |
| Red Bone Marrow | 0.12 | 0.12 | 0.12 |
| Colon | – | 0.12 | 0.12 |
| Lung | 0.12 | 0.12 | 0.12 |
| Stomach | – | 0.12 | 0.12 |
| Breasts | 0.15 | 0.05 | 0.12 |
| Bladder | – | 0.05 | 0.04 |
| Liver | – | 0.05 | 0.04 |
| Oesophagus | – | 0.05 | 0.04 |
| Thyroid | 0.03 | 0.05 | 0.04 |
| Skin | – | 0.01 | 0.01 |
| Bone surface | 0.03 | 0.01 | 0.01 |
| Salivary glands | – | – | 0.01 |
| Brain | – | – | 0.01 |
| Remainder of body | 0.30 | 0.05 | 0.12 |
| Total | 1.00 | 1.00 | 1.00 |
Calculating from the equivalent dose:
- .
Calculating from the absorbed dose:
Where
- is the effective dose to the entire organism
- is the equivalent dose absorbed by tissue T
- is the tissue weighting factor defined by regulation
- is the radiation weighting factor defined by regulation
- is the mass-averaged absorbed dose in tissue T by radiation type R
- is the absorbed dose from radiation type R as a function of location
- is the density as a function of location
- is volume
- is the tissue or organ of interest
The ICRP tissue weighting factors are chosen to represent the fraction of health risk, or biological effect, which is attributable to the specific tissue named. These weighting factors have been revised twice, as shown in the chart above.
The United States Nuclear Regulatory Commission still uses the ICRP's 1977 tissue weighting factors in their regulations, despite the ICRP's later revised recommendations.[15]
By medical imaging type
| Target organs | Exam type | Effective dose in adults[16] | Equivalent time of background radiation[16] |
|---|---|---|---|
| CT of the head | Single series | 2 mSv | 8 months |
| With + without radiocontrast | 4 mSv | 16 months | |
| Chest | CT of the chest | 7 mSv | 2 years |
| CT of the chest, lung cancer screening protocol | 1.5 mSv | 6 months | |
| Chest X-ray | 0.1 mSv | 10 days | |
| Heart | Coronary CT angiography | 12 mSv | 4 years |
| Coronary CT calcium scan | 3 mSv | 1 year | |
| Abdominal | CT of abdomen and pelvis | 10 mSv | 3 years |
| CT of abdomen and pelvis, low dose protocol | 3 mSv[17] | 1 year | |
| CT of abdomen and pelvis, with + without radiocontrast | 20 mSv | 7 years | |
| CT Colonography | 6 mSv | 2 years | |
| Intravenous pyelogram | 3 mSv | 1 year | |
| Upper gastrointestinal series | 6 mSv | 2 years | |
| Lower gastrointestinal series | 8 mSv | 3 years | |
| Spine | Spine X-ray | 1.5 mSv | 6 months |
| CT of the spine | 6 mSv | 2 years | |
| Extremities | X-ray of extremity | 0.001 mSv | 3 hours |
| Lower extremity CT angiography | 0.3 - 1.6 mSv[18] | 5 weeks - 6 months | |
| Dental X-ray | 0.005 mSv | 1 day | |
| DEXA (bone density) | 0.001 mSv | 3 hours | |
| PET-CT combination | 25 mSv | 8 years | |
| Mammography | 0.4 mSv | 7 weeks | |
Health effects
Ionizing radiation is generally harmful and potentially lethal to living things but can have health benefits in radiation therapy for the treatment of cancer and thyrotoxicosis. Its most common impact is the induction of cancer with a latent period of years or decades after exposure. High doses can cause visually dramatic radiation burns, and/or rapid fatality through acute radiation syndrome. Controlled doses are used for medical imaging and radiotherapy.
Regulatory nomenclature
UK regulations
The UK Ionising Radiations Regulations 1999 defines its usage of the term effective dose; "Any reference to an effective dose means the sum of the effective dose to the whole body from external radiation and the committed effective dose from internal radiation."[19]
US effective dose equivalent
The US Nuclear Regulatory Commission has retained in the US regulation system the older term effective dose equivalent to refer to a similar quantity to the ICRP effective dose. The NRC's total effective dose equivalent (TEDE) is the sum of external effective dose with internal committed dose; in other words all sources of dose.
In the US, cumulative equivalent dose due to external whole-body exposure is normally reported to nuclear energy workers in regular dosimetry reports.
- deep-dose equivalent, (DDE) which is properly a whole-body equivalent dose
- shallow dose equivalent, (SDE) which is actually the effective dose to the skin
History
The concept of effective dose was introduced in 1975 by Wolfgang Jacobi (1928–2015) in his publication "The concept of an effective dose: a proposal for the combination of organ doses".[6][20] It was quickly included in 1977 as “effective dose equivalent” into Publication 26 by the ICRP. In 1991, ICRP publication 60 shortened the name to "effective dose."[21] This quantity is sometimes incorrectly referred to as the "dose equivalent" because of the earlier name, and that misnomer in turn causes confusion with equivalent dose. The tissue weighting factors were revised in 1990 and 2007 due to new data.
Future use of Effective Dose
At the ICRP 3rd International Symposium on the System of Radiological Protection in October 2015, ICRP Task Group 79 reported on the "Use of Effective Dose as a Risk-related Radiological Protection Quantity".
This included a proposal to discontinue use of equivalent dose as a separate protection quantity. This would avoid confusion between equivalent dose, effective dose and dose equivalent, and to use absorbed dose in Gy as a more appropriate quantity for limiting deterministic effects to the eye lens, skin, hands & feet.[22]
It was also proposed that effective dose could be used as a rough indicator of possible risk from medical examinations. These proposals will need to go through the following stages:
- Discussion within ICRP Committees
- Revision of report by Task Group
- Reconsideration by Committees and Main Commission
- Public Consultation
See also
References
- 1 2 ICRP publication, 103 para 103
- ↑ ICRP publication 103, glossary
- ↑ ICRP publication 103, para 104 and 105
- ↑ ICRP publication 103
- ↑ ICRP report 103 para 104 and 105
- 1 2 Journal of Radiological protection Vol.35 No.3 2015. "Obituary - Wolfgang Jacobi 1928 - 2015."
- ↑ ICRP publication 103 executive summary para 101
- ↑ ICRP publication 103 executive summary para j
- ↑ ICRP publication 103 para 101
- ↑ ICRP publication 103, para 22 & glossary
- ↑ ICRP publication 103 - Glossary.
- ↑ UNSCEAR-2008 Annex A page 40, table A1, retrieved 2011-7-20
- ↑ Vennart, J. (1991). "1990 Recommendations of the International Commission on Radiological Protection". Annals of the ICRP. ICRP publication 60. 21 (1–3): 8. Bibcode:1991JRP....11..199V. doi:10.1016/0146-6453(91)90066-P. ISBN 978-0-08-041144-6.
- ↑ "The 2007 Recommendations of the International Commission on Radiological Protection". Annals of the ICRP. ICRP publication 103. 37 (2–4). 2007. ISBN 978-0-7020-3048-2. Archived from the original on 16 November 2012. Retrieved 17 May 2012.
- ↑ 10 CFR 20.1003. US Nuclear Regulatory Commission. 2009. Retrieved 25 November 2012.
- 1 2 Unless otherwise specified in boxes, reference is:
- "Radiation Dose in X-Ray and CT Exams". RadiologyInfo.org by Radiological Society of North America. Retrieved 2017-10-23. - ↑ Brisbane, Wayne; Bailey, Michael R.; Sorensen, Mathew D. (2016). "An overview of kidney stone imaging techniques". Nature Reviews Urology (Review article). Springer Nature. 13 (11): 654–662. doi:10.1038/nrurol.2016.154. ISSN 1759-4812. PMC 5443345. PMID 27578040.
- ↑ Zhang, Zhuoli; Qi, Li; Meinel, Felix G.; Zhou, Chang Sheng; Zhao, Yan E.; Schoepf, U. Joseph; Zhang, Long Jiang; Lu, Guang Ming (2014). "Image Quality and Radiation Dose of Lower Extremity CT Angiography Using 70 kVp, High Pitch Acquisition and Sinogram-Affirmed Iterative Reconstruction". PLOS ONE. 9 (6): e99112. Bibcode:2014PLoSO...999112Q. doi:10.1371/journal.pone.0099112. ISSN 1932-6203. PMC 4051648. PMID 24915439.
- ↑ The UK Ionising Radiations Regulations 1999
- ↑ Jacobi W (1975). "The concept of effective dose - A proposal for the combination of organ doses". Radiat. Environ. Biophys. 12 (2): 101–109. doi:10.1007/BF01328971. PMID 1178826. S2CID 44791936.
- ↑ ICRP publication 103 paragraph 101
- ↑ "Use of Effective Dose", John Harrison. 3rd International Symposium on the System of Radiological Protection, October 2015, Seoul.
External links
M.A. Boyd. "The Confusing World of Radiation Dosimetry - 9444" (PDF). US Environmental Protection Agency. Archived from the original (PDF) on 2016-12-21. Retrieved 2014-05-26. – an account of chronological differences between USA and ICRP dosimetry systems