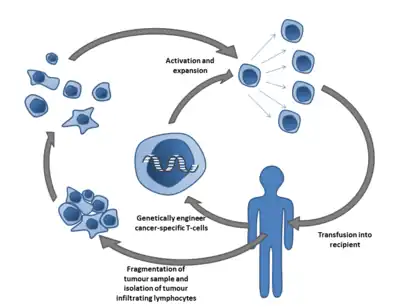
Cell therapy (also called cellular therapy, cell transplantation, or cytotherapy) is a therapy in which viable cells are injected, grafted or implanted into a patient in order to effectuate a medicinal effect,[1] for example, by transplanting T-cells capable of fighting cancer cells via cell-mediated immunity in the course of immunotherapy, or grafting stem cells to regenerate diseased tissues.
Cell therapy originated in the nineteenth century when scientists experimented by injecting animal material in an attempt to prevent and treat illness.[2] Although such attempts produced no positive benefit, further research found in the mid twentieth century that human cells could be used to help prevent the human body rejecting transplanted organs, leading in time to successful bone marrow transplantation as has become common practice in treatment for patients that have compromised bone marrow after disease, infection, radiation or chemotherapy.[3] In recent decades, however, stem cell and cell transplantation has gained significant interest by researchers as a potential new therapeutic strategy for a wide range of diseases, in particular for degenerative and immunogenic pathologies.
Background

Cell therapy can be defined as therapy in which cellular material is injected or otherwise transplanted into a patient.[1] The origins of cell therapy can perhaps be traced to the nineteenth century, when Charles-Édouard Brown-Séquard (1817–1894) injected animal testicle extracts in an attempt to stop the effects of aging.[2] In 1931 Paul Niehans (1882–1971) – who has been called the inventor of cell therapy – attempted to cure a patient by injecting material from calf embryos.[1] Niehans claimed to have treated many people for cancer using this technique, though his claims have never been validated by research.[1]
In 1953 researchers found that laboratory animals could be helped not to reject organ transplants by pre-inoculating them with cells from donor animals; in 1968, in Minnesota, the first successful human bone marrow transplantation took place.[3] In more recent work, cell encapsulation is pursued as a means to shield therapeutic cells from the host immune response. Recent work includes micro-encapsulating cells in a gel core surrounded by a solid, but permeable, shell.[4]
Bone marrow transplants are the most common and well established cell transplantation therapies. The first recording of a successful bone marrow transplant, dates back to 1956 by dr. E Donnall Thomas, who treated a leukemia patient with their twin-siblings bone marrow.[5] In general, for patients presenting damaged or destroyed bone marrow, for example after chemotherapy and/or radiation for acute myeloid leukemia (AML), bone marrow derived cells can be infused into the patients blood stream. Here the injected cells are able to home into the affected bone marrow, integrate, proliferate and recover or re-establish its biological function e.g. the haematopoiesis. Annually an estimated 18,000 patients require potentially life-saving bone marrow transplants in the US.[6] For a long time, bone marrow transplantation was the only clinically applicable method of cell transplantation, however, since the 1990s, cell therapy has been investigated for a wide scale of pathologies and disorders. Cell therapy provided a novel approach to effectuate therapeutic efficacy. Previously, medical agents could only be effective by directing and inducing the patients own cells. However, in many diseases and disorders, cell are compromised by e.g. senescence, limited blood supply (ischemia), inflammation, or simply a reduction in the number of cells. Cell therapy offers a new strategy that supports the introduction of new and active cells to restore previously compromised or deteriorated tissue- and organ structures. As such, in recent times, cell therapy has been recognized as an important field in the treatment of human disease,[7] and investigations are ongoing in articular cartilage,[8] brain tissue,[9] spine,[10] heart,[11] cancers,[12] etc. As a consequence cell therapy as a strategy has been attracting significant investments by commercial entities which suggest strong prospects for future growth.[13][14]
In 2021 Atara biotherapeutics became the first ever allogeneic T cell therapy company to be reviewed by any regulatory agency in the world (EMA)
Mechanisms of action
Cell therapy is targeted at many clinical indications in multiple organs and by several modes of cell delivery. Accordingly, the specific mechanisms of action involved in the therapies are wide-ranging. However, there are two main principles by which cells facilitate therapeutic action:
- Stem, progenitor, or mature cell engraftment, differentiation, and long-term replacement of damaged tissue. In this paradigm multipotent or unipotent cells differentiate into a specific cell type in the lab or after reaching the site of injury (via local or systemic administration). These cells then integrate into the site of injury, replacing damaged tissue, and thus facilitate improved function of the organ or tissue. An example of this is the use of cells to replace cardiomyocytes after myocardial infarction,[15][16] to facilitate angiogenesis in ischemic limb disease,[17] or the production of cartilage matrix in intervertebral disc degeneration.[18][19]
- Cells that have the capacity to release soluble factors such as cytokines, chemokines, and growth factors which act in a paracrine or endocrine manner. These factors facilitate self-healing of the organ or region by inducing local (stem) cells or attracting cells to migrate towards the transplantation site. Early cell passages have been shown to be more efficient paracrine activity than later passages.[20][21] The delivered cells (via local or systemic administration) remain viable for a relatively short period (days-weeks) and then die. This includes cells that naturally secrete the relevant therapeutic factors, or which undergo epigenetic changes or genetic engineering that causes the cells to release large quantities of a specific molecule. Examples of this include cells that secrete factors which facilitate angiogenesis, anti-inflammation, and anti-apoptosis.[22][23][24] This mode of action is proposed by companies such as Pluristem and Pervasis that use adherent stromal cells or mature endothelial cells to treat peripheral artery disease and arteriovenous access complications.[25][26]
Cell therapy strategies
Allogeneic
In allogeneic cell therapy the donor is a different person to the recipient of the cells.[27] In pharmaceutical manufacturing, the allogenic methodology is promising because unmatched allogenic therapies can form the basis of "off the shelf" products.[28] There is research interest in attempting to develop such products to treat conditions including Crohn's disease[29] and a variety of vascular conditions.[30]
Autologous
In autologous cell therapy, cells are transplanted that are derived from the patients own tissues. Multiple clinical studies are ongoing that obtain stromal cells from bone-marrow, adipose tissue, or peripheral blood to be transplanted at sites of injury or stress; which is being actively explored for e.g. cartilage[31] and muscle[32] repair. It could also involve the isolation of matured cells from diseased tissues, to be later re-implanted at the same or neighboring tissues; a strategy being assessed in clinical trials for e.g. the spine in preventing disc reherniation or adjacent disc disease.[33][34] The benefit of an autologous strategy is that there is limited concern for immunogenic responses or transplant rejection. Nevertheless, an autologous strategy is often costly due to patient-by-patient processing, thus preventing the option to create large quality-controlled batches. Moreover, autologous strategies generally do not allow for product quality and effectiveness testing prior to transplantation, as it is highly donor (thus patient) dependent. This is a particular concern as often the patient functioning as donor is diseased, and this can impact cell potency and quality.
Xenogeneic
In xenogeneic cell therapies, the recipient will receive cells from another species. For example, the transplantation of pig derived cells to humans. Currently, xenogeneic cell therapies primarily involve human cell transplantation into experimental animal models for assessment of efficacy and safety,[17] however future advances could potentially enable xenogeneic strategies to humans as well.[35]
Types of cells
Human embryonic stem cells
Research into human embryonic stem cells is controversial, and regulation varies from country to country, with some countries banning it outright. Nevertheless, these cells are being investigated as the basis for a number of therapeutic applications, including possible treatments for diabetes[36] and Parkinson's disease.[37]
Neural stem cell therapy
Neural stem cells (NSCs) are the subject of ongoing research for possible therapeutic applications, for example for treating a number of neurological disorders such as Parkinson's disease and Huntington's disease.[38]
Mesenchymal stem cell therapy
MSCs are immunomodulatory, multipotent and fast proliferating and these unique capabilities mean they can be used for a wide range of treatments including immune-modulatory therapy, bone and cartilage regeneration, myocardium regeneration and the treatment of Hurler syndrome, a skeletal and neurological disorder.[39]
Researchers have demonstrated the use of MSCs for the treatment of osteogenesis imperfecta (OI). Horwitz et al. transplanted bone marrow (BM) cells from human leukocyte antigen (HLA)-identical siblings to patients with OI. Results show that MSCs can develop into normal osteoblasts, leading to fast bone development and reduced fracture frequencies.[40] A more recent clinical trial showed that allogeneic fetal MSCs transplanted in utero in patients with severe OI can engraft and differentiate into bone in a human fetus.[41]
Besides bone and cartilage regeneration, cardiomyocyte regeneration with autologous BM MSCs has also been reported recently. Introduction of BM MSCs following myocardial infarction (MI) resulted in significant reduction of damaged regions and improvement in heart function. Clinical trials for treatment of acute MI with Prochymal by Osiris Therapeutics are underway. Also, a clinical trial revealed huge improvements in nerve conduction velocities in Hurler's Syndrome patients infused with BM MSCs from HLA-identical siblings.[42]
Hematopoietic stem cell transplantation
Hematopoietic stem cells (HSCs), derived from bone marrow or blood, are cells with the abilities to self-renew and to differentiate into all types of blood cells, especially those involved in the human immune system. Thus, they can be used to treat blood and immune disorders. Since human bone marrow grafting was first published in 1957,[43] there have been significant advancements in HSCs therapy. Following that, syngeneic marrow infusion[44] and allogeneic marrow grafting[45] were performed successfully. HSCs therapy can also render its cure by reconstituting damaged blood-forming cells and restoring the immune system after high-dose chemotherapy to eliminate disease.[46]
There are three types of HSC transplantation: syngeneic, autologous, and allogeneic transplants.[39] Syngeneic transplantations occur between identical twins. Autologous transplantations use the HSCs obtained directly from the patient and hence avoid complications of tissue incompatibility; whereas allogeneic transplantations involve the use of donor HSCs, either genetically related or unrelated to the recipient. To lower the risks of transplant, which include graft rejection and graft-versus-host disease (GVHD), allogeneic HSCT must satisfy compatibility at the HLA loci (i.e. genetic matching to reduce the immunogenicity of the transplant).
In addition to bone marrow-derived HSCs, the use of alternative sources such as umbilical cord blood (UCB) and peripheral blood stem cells (PBSCs) has been increasing. In comparison with bone marrow-derived HSC recipients, PBSC recipients who had myeloid malignancies reported a faster engraftment and better overall survival.[47] The use of UCB requires less stringent HLA loci matching, although the time of engraftment is longer and graft failure rate is higher.[48][49]
Differentiated or mature cell transplantation
Alternative to stem- or progenitor cells, investigations are exploring the transplantation of differentiated cells that only possess low or no proliferation ability. This tends to involve specialized cells able to facilitate specific function in the patients body (for example, transplantation of cardiomyocytes[50] to repair heart function or islet cell transplantation[51] for establishing insulin homeostasis in diabetes patients) or support/regenerate the extracellular matrix production of specific tissues (for example intervertebral disc repair by transplanting chondrocytes[10]).
Alternative medicine
In alternative medicine, cell therapy is defined as the injection of non-human cellular animal material in an attempt to treat illness.[1] Quackwatch labels this as "senseless", since "cells from the organs of one species cannot replace the cells from the organs of other species" and because a number of serious adverse effects have been reported.[52] Of this alternative, animal-based form of cell therapy, the American Cancer Society say: "Available scientific evidence does not support claims that cell therapy is effective in treating cancer or any other disease. It may in fact be lethal ...".[1]
Manufacturing
Despite being one of the fast growing areas within Life Sciences,[53] the manufacturing of cell therapy products is largely hindered by small scale batches and labour-intensive processes.[54]
A number of manufacturers are turning to automated methods of production, eliminating human involvement and risk of human error. Automated methods of cell therapy manufacturing have opened up larger scale production of higher quality products at lower cost.[55]
Supply chain
Logistics departments of biopharma companies experience new obstacles because of the introduction of new cell and gene therapy products, such as CAR T-cell therapies and allogeneic therapies. Cell and gene therapies require manufacturer and distributors alike to implement new systems and processes in order to ensure safe handling and delivery. Additionally, on-demand inventory therefore becomes more and more important, especially with regard to unforeseeable events like the COVID-19 pandemic, so that supply chain interruptions can be prevented.[56] Furthermore recent changes as a result of the COVID 19 pandemic and political instability in Europe, secondary to Brexit, have further impacted the logistics chain for cellular therapies. [57]
See also
References
- 1 2 3 4 5 6 "Cell Therapy". American Cancer Society. 1 November 2008. Archived from the original on 26 April 2015. Retrieved 15 September 2013.
- 1 2 Lefrère JJ, Berche P (March 2010). "[Doctor Brown-Sequard's therapy]". Annales d'Endocrinologie. 71 (2): 69–75. doi:10.1016/j.ando.2010.01.003. PMID 20167305.
- 1 2 Starzl TE (July 2000). "History of clinical transplantation". World Journal of Surgery. 24 (7): 759–782. doi:10.1007/s002680010124. PMC 3091383. PMID 10833242.
- ↑ Zhou X, Haraldsson T, Nania S, Ribet F, Palano G, Heuchel R, Löhr M, van der Wijngaart W (2018). "Human Cell Encapsulation in Gel Microbeads with Cosynthesized Concentric Nanoporous Solid Shells". Adv. Funct. Mater. 28 (21): 1707129. doi:10.1002/adfm.201707129. hdl:10616/47027. S2CID 104267420.
- ↑ "Australian Cancer Research Foundation". Home.cancerresearch. 2014-12-07. Archived from the original on 2020-02-02. Retrieved 2020-03-22.
- ↑ "Health Resources & Services Administration". HRSA.gov. 2020-03-21.
- ↑ Gage FH (April 1998). "Cell therapy". Nature. 392 (6679 Suppl): 18–24. PMID 9579857.
- ↑ Fuggle NR, Cooper C, Oreffo RO, Price AJ, Kaux JF, Maheu E, et al. (April 2020). "Alternative and complementary therapies in osteoarthritis and cartilage repair". Aging Clinical and Experimental Research. 32 (4): 547–560. doi:10.1007/s40520-020-01515-1. PMC 7170824. PMID 32170710.
- ↑ Henchcliffe C, Parmar M (2018-12-18). Brundin P, Langston JW, Bloem BR (eds.). "Repairing the Brain: Cell Replacement Using Stem Cell-Based Technologies". Journal of Parkinson's Disease. 8 (s1): S131–S137. doi:10.3233/JPD-181488. PMC 6311366. PMID 30584166.
- 1 2 Schol J, Sakai D (April 2019). "Cell therapy for intervertebral disc herniation and degenerative disc disease: clinical trials". International Orthopaedics. 43 (4): 1011–1025. doi:10.1007/s00264-018-4223-1. PMID 30498909. S2CID 53981159.
- ↑ Jing D, Parikh A, Canty JM, Tzanakakis ES (December 2008). "Stem cells for heart cell therapies". Tissue Engineering. Part B, Reviews. 14 (4): 393–406. doi:10.1089/ten.teb.2008.0262. PMC 2710610. PMID 18821841.
- ↑ Guedan S, Ruella M, June CH (April 2019). "Emerging Cellular Therapies for Cancer". Annual Review of Immunology. 37 (1): 145–171. doi:10.1146/annurev-immunol-042718-041407. PMC 7399614. PMID 30526160.
- ↑ Brindley DA, Reeve BC, Sahlman WA, Bonfiglio GA, Davie NL, Culme-Seymour EJ, Mason C (November 2011). "The impact of market volatility on the cell therapy industry". Cell Stem Cell. 9 (5): 397–401. doi:10.1016/j.stem.2011.10.010. PMID 22056137.
- ↑ Mason C, Brindley DA, Culme-Seymour EJ, Davie NL (May 2011). "Cell therapy industry: billion dollar global business with unlimited potential". Regenerative Medicine. 6 (3): 265–272. doi:10.2217/rme.11.28. PMID 21548728.
- ↑ Jackson KA, Majka SM, Wang H, Pocius J, Hartley CJ, Majesky MW, et al. (June 2001). "Regeneration of ischemic cardiac muscle and vascular endothelium by adult stem cells". The Journal of Clinical Investigation. 107 (11): 1395–1402. doi:10.1172/jci12150. PMC 209322. PMID 11390421.
- ↑ Kawada H, Fujita J, Kinjo K, Matsuzaki Y, Tsuma M, Miyatake H, et al. (December 2004). "Nonhematopoietic mesenchymal stem cells can be mobilized and differentiate into cardiomyocytes after myocardial infarction". Blood. 104 (12): 3581–3587. doi:10.1182/blood-2004-04-1488. PMID 15297308.
- 1 2 Kalka C, Masuda H, Takahashi T, Kalka-Moll WM, Silver M, Kearney M, et al. (March 2000). "Transplantation of ex vivo expanded endothelial progenitor cells for therapeutic neovascularization". Proceedings of the National Academy of Sciences of the United States of America. 97 (7): 3422–3427. Bibcode:2000PNAS...97.3422K. doi:10.1073/pnas.97.7.3422. PMC 16255. PMID 10725398.
- ↑ Hiraishi S, Schol J, Sakai D, Nukaga T, Erickson I, Silverman L, et al. (June 2018). "Discogenic cell transplantation directly from a cryopreserved state in an induced intervertebral disc degeneration canine model". JOR Spine. 1 (2): e1013. doi:10.1002/jsp2.1013. PMC 6686803. PMID 31463441.
- ↑ Wang W, Deng G, Qiu Y, Huang X, Xi Y, Yu J, et al. (May 2018). "Transplantation of allogenic nucleus pulposus cells attenuates intervertebral disc degeneration by inhibiting apoptosis and increasing migration". International Journal of Molecular Medicine. 41 (5): 2553–2564. doi:10.3892/ijmm.2018.3454. PMC 5846671. PMID 29436582.
- ↑ "2017 TERMIS - Americas Conference & Exhibition Charlotte, NC December 3-6, 2017". Tissue Engineering. Part A. 23 (S1): S1–S159. December 2017. doi:10.1089/ten.tea.2017.29003.abstracts. hdl:1842/35967. PMID 29173019. S2CID 146034988.
- ↑ von Bahr L, Sundberg B, Lönnies L, Sander B, Karbach H, Hägglund H, et al. (April 2012). "Long-term complications, immunologic effects, and role of passage for outcome in mesenchymal stromal cell therapy". Biology of Blood and Marrow Transplantation. 18 (4): 557–564. doi:10.1016/j.bbmt.2011.07.023. PMID 21820393.
- ↑ Deuse, T., C. Peter, et al. (2009). "Hepatocyte growth factor or vascular endothelial growth factor gene transfer maximizes mesenchymal stem cell-based myocardial salvage after acute myocardial infarction." Circulation 120(11 Suppl): S247–54.
- ↑ Kelly ML, Wang M, Crisostomo PR, Abarbanell AM, Herrmann JL, Weil BR, Meldrum DR (June 2010). "TNF receptor 2, not TNF receptor 1, enhances mesenchymal stem cell-mediated cardiac protection following acute ischemia". Shock. 33 (6): 602–607. doi:10.1097/shk.0b013e3181cc0913. PMC 3076044. PMID 19953003.
- ↑ Yagi H, Soto-Gutierrez A, Parekkadan B, Kitagawa Y, Tompkins RG, Kobayashi N, Yarmush ML (2010). "Mesenchymal stem cells: Mechanisms of immunomodulation and homing". Cell Transplantation. 19 (6): 667–679. doi:10.3727/096368910x508762. PMC 2957533. PMID 20525442.
- ↑ Nugent HM, Ng YS, White D, Groothius A, Kanner G, Edelman ER (December 2009). "Delivery site of perivascular endothelial cell matrices determines control of stenosis in a porcine femoral stent model". Journal of Vascular and Interventional Radiology. 20 (12): 1617–1624. doi:10.1016/j.jvir.2009.08.020. PMC 2788031. PMID 19854069.
- ↑ Prather WR, Toren A, Meiron M, Ofir R, Tschope C, Horwitz EM (2009). "The role of placental-derived adherent stromal cell (PLX-PAD) in the treatment of critical limb ischemia". Cytotherapy. 11 (4): 427–434. doi:10.1080/14653240902849762. PMID 19526389.
- ↑ "Allogeneic Stem Cell Transplant". WebMD. Retrieved 15 September 2013.
- ↑ Brandenberger R, Burger S, Campbell A, Fong T, Lapinskas E, Rowley JA (2011). "Cell Therapy Bioprocessing: Integrating Process and Product Development for the Next Generation of Biotherapeutics" (PDF). BioProcess International. 9 (suppl. I): 30–37.
- ↑ Newman RE, Yoo D, LeRoux MA, Danilkovitch-Miagkova A (June 2009). "Treatment of inflammatory diseases with mesenchymal stem cells". Inflammation & Allergy - Drug Targets. 8 (2): 110–123. CiteSeerX 10.1.1.323.3687. doi:10.2174/187152809788462635. PMID 19530993.
- ↑ Mays RW, van't Hof W, Ting AE, Perry R, Deans R (February 2007). "Development of adult pluripotent stem cell therapies for ischemic injury and disease". Expert Opinion on Biological Therapy. 7 (2): 173–184. doi:10.1517/14712598.7.2.173. PMID 17250456. S2CID 22258887.
- ↑ Yamasaki S, Mera H, Itokazu M, Hashimoto Y, Wakitani S (October 2014). "Cartilage Repair With Autologous Bone Marrow Mesenchymal Stem Cell Transplantation: Review of Preclinical and Clinical Studies". Cartilage. 5 (4): 196–202. doi:10.1177/1947603514534681. PMC 4335770. PMID 26069698.
- ↑ Linard C, Brachet M, L'homme B, Strup-Perrot C, Busson E, Bonneau M, et al. (November 2018). "Long-term effectiveness of local BM-MSCs for skeletal muscle regeneration: a proof of concept obtained on a pig model of severe radiation burn". Stem Cell Research & Therapy. 9 (1): 299. doi:10.1186/s13287-018-1051-6. PMC 6225585. PMID 30409227.
- ↑ Mochida J, Sakai D, Nakamura Y, Watanabe T, Yamamoto Y, Kato S (March 2015). "Intervertebral disc repair with activated nucleus pulposus cell transplantation: a three-year, prospective clinical study of its safety". European Cells & Materials. 29: 202–12, discussion 212. doi:10.22203/eCM.v029a15. PMID 25794529.
- ↑ Meisel HJ, Ganey T, Hutton WC, Libera J, Minkus Y, Alasevic O (August 2006). "Clinical experience in cell-based therapeutics: intervention and outcome". European Spine Journal. 15 (Suppl 3): S397–S405. doi:10.1007/s00586-006-0169-x. PMC 2335385. PMID 16850291.
- ↑ Zhong R, Platt JL (November 2005). "Current status of animal-to-human transplantation". Expert Opinion on Biological Therapy. 5 (11): 1415–1420. doi:10.1517/14712598.5.11.1415. PMC 1475507. PMID 16255645.
- ↑ D'Amour KA, Bang AG, Eliazer S, Kelly OG, Agulnick AD, Smart NG, et al. (November 2006). "Production of pancreatic hormone-expressing endocrine cells from human embryonic stem cells". Nature Biotechnology. 24 (11): 1392–1401. doi:10.1038/nbt1259. PMID 17053790. S2CID 11040949.
- ↑ Parish CL, Arenas E (2007). "Stem-cell-based strategies for the treatment of Parkinson's disease". Neuro-Degenerative Diseases. 4 (4): 339–347. doi:10.1159/000101892. PMID 17627139. S2CID 37229348.
- ↑ Bonnamain V, Neveu I, Naveilhan P (2012). "Neural stem/progenitor cells as a promising candidate for regenerative therapy of the central nervous system". Frontiers in Cellular Neuroscience. 6: 17. doi:10.3389/fncel.2012.00017. PMC 3323829. PMID 22514520.
- 1 2 Oh SKW and Choo ABH (2011) "The Biological Basis | Stem Cells". In: Murray Moo-Young (ed.), Comprehensive Biotechnology, Second Edition, Volume 1, pp. 341–65. Elsevier.
- ↑ Horwitz EM, Prockop DJ, Fitzpatrick LA, Koo WW, Gordon PL, Neel M, et al. (March 1999). "Transplantability and therapeutic effects of bone marrow-derived mesenchymal cells in children with osteogenesis imperfecta". Nature Medicine. 5 (3): 309–313. doi:10.1038/6529. PMID 10086387. S2CID 38011739.
- ↑ Le Blanc K, Götherström C, Ringdén O, Hassan M, McMahon R, Horwitz E, et al. (June 2005). "Fetal mesenchymal stem-cell engraftment in bone after in utero transplantation in a patient with severe osteogenesis imperfecta". Transplantation. 79 (11): 1607–1614. doi:10.1097/01.tp.0000159029.48678.93. PMID 15940052. S2CID 7040451.
- ↑ Koç ON, Day J, Nieder M, Gerson SL, Lazarus HM, Krivit W (August 2002). "Allogeneic mesenchymal stem cell infusion for treatment of metachromatic leukodystrophy (MLD) and Hurler syndrome (MPS-IH)". Bone Marrow Transplantation. 30 (4): 215–222. doi:10.1038/sj.bmt.1703650. PMID 12203137.
- ↑ Thomas ED, Lochte HL, Cannon JH, Sahler OD, Ferrebee JW (October 1959). "Supralethal whole body irradiation and isologous marrow transplantation in man". The Journal of Clinical Investigation. 38 (10 Pt 1-2): 1709–1716. doi:10.1172/jci103949. PMC 444138. PMID 13837954.
- ↑ Van Den Berg DJ, Sharma AK, Bruno E, Hoffman R (November 1998). "Role of members of the Wnt gene family in human hematopoiesis". Blood. 92 (9): 3189–3202. doi:10.1182/blood.V92.9.3189. PMID 9787155. S2CID 227264894.
- ↑ Wilson A, Trumpp A (February 2006). "Bone-marrow haematopoietic-stem-cell niches". Nature Reviews. Immunology. 6 (2): 93–106. doi:10.1038/nri1779. PMID 16491134. S2CID 205489817.
- ↑ Hwang WY (September 2004). "Haematopoietic graft engineering". Annals of the Academy of Medicine, Singapore. 33 (5): 551–558. PMID 15531949.
- ↑ Bhardwaj G, Murdoch B, Wu D, Baker DP, Williams KP, Chadwick K, et al. (February 2001). "Sonic hedgehog induces the proliferation of primitive human hematopoietic cells via BMP regulation". Nature Immunology. 2 (2): 172–180. doi:10.1038/84282. PMID 11175816. S2CID 27907370.
- ↑ Sharma S, Gurudutta GU, Satija NK, Pati S, Afrin F, Gupta P, et al. (December 2006). "Stem cell c-KIT and HOXB4 genes: critical roles and mechanisms in self-renewal, proliferation, and differentiation". Stem Cells and Development. 15 (6): 755–778. doi:10.1089/scd.2006.15.755. PMID 17253940.
- ↑ Thomas ED, Storb R (October 1970). "Technique for human marrow grafting". Blood. 36 (4): 507–515. doi:10.1182/blood.V36.4.507.507. PMID 4916999.
- ↑ Hashimoto H, Olson EN, Bassel-Duby R (October 2018). "Therapeutic approaches for cardiac regeneration and repair". Nature Reviews. Cardiology. 15 (10): 585–600. doi:10.1038/s41569-018-0036-6. PMC 6241533. PMID 29872165.
- ↑ Gamble A, Pepper AR, Bruni A, Shapiro AM (March 2018). "The journey of islet cell transplantation and future development". Islets. 10 (2): 80–94. doi:10.1080/19382014.2018.1428511. PMC 5895174. PMID 29394145.
- ↑ Barrett S (21 August 2003). "Cellular Therapy". Quackwatch. Retrieved 15 September 2013.
- ↑ "Growth in Sales of Products In Cell Therapy and Tissue Engineering". ebers Medical.
- ↑ "Scaling Up Cell Therapy Manufacturing". Genetic Engineering and Biotechnology News. 7 September 2018.
- ↑ "Cell Therapy Process Development". Next Generation Therapeutics.
- ↑ "Supply Chain Optimization in Cell and Gene Therapies". Single Use Support. 20 December 2021.
- ↑ Hennessy C, Deptula M, Hester J, Issa F (2023). "Barriers to Treg therapy in Europe: From production to regulation". Frontiers in Medicine. 10: 1090721. doi:10.3389/fmed.2023.1090721. PMC 9892909. PMID 36744143.